If you are considering refractive cataract surgery, one of the biggest questions on your mind is likely to be how accurate your vision will be afterward. When surgery is described as “refractive,” it naturally creates an expectation of precision, and many people hope for results that closely match their visual goals. Wanting reassurance about accuracy is completely reasonable when the outcome affects how you see every day.
Unlike standard cataract surgery, refractive cataract surgery places a strong emphasis on visual precision. The aim is not just to remove the cloudy lens but to fine-tune your vision as accurately as possible. Understanding how accuracy is measured, what modern technology can realistically achieve, and why small variations sometimes occur can help you set expectations that are confident and informed rather than uncertain or anxious.
This article walks you through what vision accuracy truly means after refractive cataract surgery, how surgeons plan for precise outcomes, and what options exist if small refinements are needed afterward. When you understand the process, accuracy becomes something you can trust rather than worry about.
What “Vision Accuracy” Really Means After Surgery

After refractive cataract surgery, vision accuracy does not mean perfect vision in an absolute sense. Instead, it refers to how closely your final visual result matches the goal that was agreed before surgery. That goal may be clear distance vision, reduced reliance on glasses, or balanced vision across different distances.
1. Accuracy Means Hitting the Planned Target – Vision accuracy is measured by how close your final prescription is to the intended outcome. This helps surgeons assess how successfully the surgical plan has been achieved.
2. Zero Prescription Is Not Always the Goal – Being “accurate” does not necessarily mean having no prescription at all. Some patients intentionally choose a small amount of focus to support specific visual needs, such as reading or intermediate tasks.
3. Vision Quality Goes Beyond Numbers – Vision accuracy is not only about prescription values. Comfort, stability, contrast, and clarity in real-world conditions all influence how accurate your vision feels in everyday life.
Ultimately, the success of surgery is judged not just by measurements, but by how well your vision supports your daily activities. Understanding this broader definition of accuracy helps set realistic expectations and improves overall satisfaction with the outcome.
How Accuracy Is Planned Before Refractive Cataract Surgery
Achieving accurate visual results starts well before the day of surgery. Pre-operative planning is the most important stage in refractive cataract surgery, as it determines how precisely your vision can be corrected. Detailed measurements and careful analysis guide every decision, forming the foundation for predictable outcomes. This planning ensures surgery is tailored to your eyes rather than based on averages.
- Advanced biometry measurements – Modern technology measures eye length, corneal curvature, and internal eye relationships with high precision.
- Accurate lens power calculation – These detailed measurements are used to calculate the ideal intraocular lens power.
- Assessment of astigmatism – Corneal shape and astigmatism are carefully analysed to guide correction strategies.
- Consideration of eye health – Existing eye conditions are factored in to ensure safe and realistic outcomes.
- Personalised visual goals – Planning reflects how you want to use your vision in daily life, not just numerical targets.
Accuracy in refractive cataract surgery is both technical and personal. By combining precise measurements with an understanding of your visual needs, surgeons aim to deliver results that feel natural, reliable, and aligned with real-world vision expectations.
The Role of Modern Biometry in Accuracy

Biometry is the technology that measures your eye before surgery. Modern optical biometry devices use light rather than sound to create extremely precise measurements. These machines can measure eye length to fractions of a millimetre, which makes a meaningful difference to final vision.
Small differences in eye length can change the outcome of lens power calculations. This is why modern biometry has dramatically improved accuracy compared with older techniques. It reduces variability and increases confidence in predicted outcomes. In refractive cataract surgery, biometry is often repeated or cross-checked to ensure consistency. This extra care helps minimise error and contributes directly to accurate post-operative vision.
Lens Power Calculations and Their Precision
Selecting the correct lens power is a critical step in refractive cataract surgery. Once detailed eye measurements are taken, advanced mathematical formulas are used to plan the lens that best matches your visual target. These calculations aim to deliver the most accurate and predictable outcome possible.
1. How Lens Power Is Calculated – Modern formulas use multiple measurements, including eye length and corneal shape, to predict how the artificial lens will sit inside the eye after surgery. They are continually refined using large clinical datasets and real-world outcomes.
2. Improvements in Modern Accuracy – Today’s calculation methods are far more precise than those used even ten years ago. They perform particularly well in average-sized eyes and have also significantly improved results in eyes that are longer, shorter, or more complex.
3. Why Absolute Precision Is Not Possible – Despite advanced technology, no system can predict outcomes with complete certainty. The eye is a living structure, and small variations in healing can influence the final result.
Overall, lens power calculations deliver a very high level of accuracy, but they are not mathematically perfect in every case. Understanding this natural variability helps set realistic expectations while appreciating how reliable modern cataract surgery outcomes truly are.
How Accurate Are Typical Outcomes in Real Terms?
For most people undergoing refractive cataract surgery, vision accuracy is very high. A large proportion of patients achieve results that are extremely close to the intended target, often within a small margin that does not significantly affect daily life.
Many patients achieve excellent distance vision and reduced reliance on glasses, particularly when the surgery is planned carefully and the eyes are otherwise healthy. Accuracy has improved steadily over time as technology and surgical techniques have advanced.
However, accuracy does not mean identical results for everyone. Individual anatomy, healing patterns, and pre-existing eye conditions can all influence final vision. These differences are usually small but important to acknowledge.
Why Vision Results Can Vary Slightly
Refractive cataract surgery is highly accurate, but no surgical outcome can be predicted with absolute precision. Even with advanced planning and modern technology, small variations can occur as the eye heals and adapts after surgery. These changes are usually minor and well within expected limits. Understanding why they happen helps set realistic expectations.
- Individual healing response – Each eye heals differently, and subtle biological differences can influence final vision.
- Lens position settling – The intraocular lens may settle slightly differently than predicted during the healing process.
- Corneal healing changes – Minor shifts in corneal shape can affect focus, especially in those with astigmatism or dry eye.
- Not a surgical fault – Small variations reflect normal biological processes rather than technical errors.
- Minimal impact for most patients – In the majority of cases, differences are small and do not significantly affect vision or satisfaction.
While perfect predictability is not possible, modern refractive cataract surgery consistently delivers reliable and high-quality results. Awareness of these natural variations allows patients to approach surgery with confidence and balanced expectations.
The Impact of Astigmatism on Accuracy
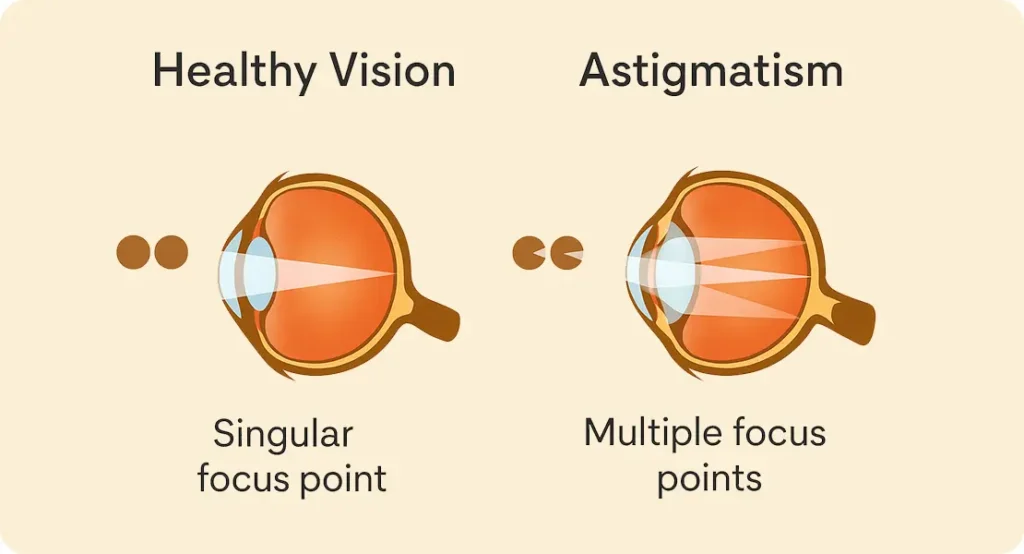
Astigmatism is an important factor influencing visual accuracy after refractive cataract surgery. Even when lens power calculations are precise, uncorrected or under-corrected astigmatism can limit sharpness and clarity. Managing astigmatism effectively is therefore essential for achieving the intended visual outcome.
1. How Astigmatism Affects Vision Accuracy – If astigmatism is present and not fully corrected, vision may remain blurred or distorted. This can occur despite otherwise accurate lens calculations.
2. Modern Astigmatism Management Options – Refractive cataract surgery often includes astigmatism correction using toric intraocular lenses or specialised corneal techniques. Accurate measurements and precise planning are key to selecting the right approach.
3. Importance of Alignment and Surgical Precision – Small alignment shifts can significantly affect astigmatism correction. Careful pre-operative marking and surgical accuracy are therefore critical to achieving optimal results.
When astigmatism is managed well, both visual accuracy and overall clarity improve markedly. Attention to these details helps ensure that surgical outcomes align as closely as possible with the planned visual goals.
Multifocal and Extended-Range Lenses and Accuracy
Some people choose lenses designed to provide vision at multiple distances. These lenses work by splitting or extending focus rather than relying on a single focal point. Accuracy with these lenses is measured slightly differently. The goal is not a perfect single focus but a balanced range of useful vision. Small residual prescriptions may still exist, but functional vision can be excellent.
Because these lenses rely on optical design rather than pure focus, individual adaptation also plays a role. Accuracy includes how well your brain adjusts to the new visual system, not just numerical measurements.
The Difference Between Accuracy and Satisfaction
Accuracy and satisfaction are closely related but not always the same in refractive cataract surgery. A technically precise outcome does not automatically guarantee happiness with the result, just as a small residual prescription does not necessarily lead to dissatisfaction. How vision feels in daily life depends on individual priorities and expectations. Understanding this distinction is key to a positive experience.
- Different measures of success – Clinical accuracy focuses on numbers, while satisfaction reflects how vision performs in real-world situations.
- Lifestyle priorities matter – Night driving, screen use, or reading place different demands on vision and influence how results are perceived.
- Sensitivity to specific issues – Some people notice glare more, while others focus on near or distance clarity.
- Contextual interpretation of accuracy – Small residual errors may be insignificant if they do not affect daily activities.
- Expectation alignment – Clear discussions before surgery help match achievable accuracy with personal visual goals.
This is why pre-operative conversations are so important. When expectations are realistic and aligned with surgical possibilities, even minor imperfections are less likely to feel disappointing, and overall satisfaction is much higher.
Measuring Vision Accuracy After Surgery
After refractive cataract surgery, vision accuracy is assessed through a combination of vision testing and patient feedback. Refraction tests measure how close your vision is to the intended prescription. Your surgeon also asks how your vision feels in daily life. Comfort, stability, and confidence are all considered alongside test results. Accuracy is therefore both objective and subjective. Numbers matter, but how you experience your vision matters just as much.
When Vision Is Not Exactly as Planned
Occasionally, vision may not land exactly on the intended target. This does not necessarily mean the surgery has failed. Small residual prescriptions are common and often easily managed.
In many cases, the difference is so minor that it does not require any action. Glasses for specific tasks may be enough to achieve complete satisfaction.
When refinement is needed, there are safe and effective options available. Understanding this possibility in advance can reduce anxiety if outcomes are not mathematically perfect.
Enhancements and Refinement Options
Enhancements are additional procedures used to fine-tune vision after cataract surgery when small adjustments are needed. They are not routine for everyone, but they provide a way to refine results if the final vision differs slightly from the original plan.
1. Types of Enhancement Procedures – Enhancements may involve laser vision correction to adjust focus, or in rare situations, a lens adjustment or exchange. The choice depends on the type of lens used, eye health, and the nature of the remaining prescription.
2. Timing and Visual Stability – Enhancements are only considered once the eye has fully healed and vision has stabilised. This waiting period ensures that any refinement is based on reliable measurements rather than temporary changes related to healing.
3. Why Enhancements Add Flexibility – The availability of enhancement options is one reason refractive cataract surgery is considered adaptable. Rather than accepting small inaccuracies as final, surgeons can address them to better align outcomes with the intended visual goals.
When used appropriately, enhancements help optimise vision and improve satisfaction, offering reassurance that refinement is possible if needed.
How Often Are Enhancements Needed?
Most people do not need any enhancement after refractive cataract surgery. When an enhancement is required, it is usually to fine-tune a small remaining prescription rather than to correct a significant problem.
1. Typical Enhancement Rates – Thanks to modern eye measurements and improved surgical techniques, enhancement rates are relatively low. The majority of patients achieve outcomes that are close enough to their planned target that no further treatment is necessary.
2. Role of Technology and Planning – Advances in biometry, lens calculation formulas, and surgical precision have steadily reduced the need for refinement. Careful assessment before surgery, including realistic goal-setting, also helps minimise the likelihood of needing an enhancement.
3. Enhancements as a Safety Net – Knowing that enhancement options exist can be reassuring. They are best viewed as a backup rather than an expectation, offering flexibility if small adjustments are needed once healing is complete.
For most patients, surgery alone delivers satisfactory results, with enhancements reserved for occasional fine-tuning rather than routine correction.
Eye Health Factors That Affect Accuracy
Underlying eye conditions can influence accuracy. Conditions such as dry eye, corneal irregularities, or retinal issues may affect visual outcomes even when surgery is technically successful.
Managing these conditions before surgery improves accuracy. This is why thorough pre-operative assessment is essential in refractive cataract surgery.
Addressing eye health proactively helps ensure that measured accuracy translates into real-world visual satisfaction.
Age and Healing Response
Age can influence how the eye heals after cataract surgery, but it does not automatically limit accuracy or final visual outcomes. Many older patients achieve excellent, stable vision following refractive cataract surgery. What often differs is the pace of recovery rather than the quality of the result. Recognising this helps set appropriate expectations.
- Accuracy remains high – Older age alone does not prevent precise refractive outcomes or long-term visual stability.
- Healing pace may vary – Some individuals experience a slightly slower recovery as the eye settles after surgery.
- Gradual visual refinement – Vision often continues to improve over weeks rather than within a few days.
- Importance of patience – Early fluctuations are common and usually resolve as healing progresses.
- Reduced post-operative anxiety – Understanding the expected timeline helps avoid unnecessary concern in the early phase.
By appreciating how age can affect healing speed without compromising accuracy, patients can approach recovery with confidence. Allowing time for the eye to stabilise ensures a clearer understanding of the final visual outcome.
How Long It Takes for Vision to Stabilise
Vision accuracy is not fully assessed immediately after surgery. The eye needs time to heal, and vision often fluctuates during the early weeks. Most people notice significant improvement quickly, but final accuracy is usually assessed after several weeks once healing has stabilised. This timeline is normal and expected. Judging outcomes too early can lead to unnecessary concern. Stability is a key part of accurate assessment.
Setting Realistic Expectations
Refractive cataract surgery offers a high level of accuracy, but it does not promise absolute perfection. Understanding this helps you focus on meaningful improvements rather than small, unavoidable imperfections.
Accuracy is best thought of as a range rather than a single exact outcome. Within this range, most patients achieve vision that comfortably meets or even exceeds their everyday visual needs.
Open and honest communication with your surgeon is essential. When expectations are discussed clearly in advance, results are more satisfying and feel aligned with what is realistically achievable.
How Surgeon Experience Influences Accuracy
Surgeon experience plays a significant role in the accuracy of refractive cataract surgery. While advanced technology supports planning and measurements, consistent results depend heavily on how that information is interpreted and applied during surgery.
1. Managing Variables During Surgery – Surgeons who regularly perform refractive procedures are more familiar with subtle variables that can influence outcomes. This includes handling different eye anatomies, maintaining precise lens positioning, and responding effectively to intraoperative changes.
2. Judgement in Planning and Technique – Experience improves decision-making in lens selection, astigmatism management, and surgical technique. These judgements are especially important when tailoring outcomes to individual visual goals rather than aiming for a standard result.
3. Post-Operative Assessment and Refinement – Experienced surgeons are also better equipped to assess healing patterns and determine whether any refinement is needed. This contributes to stable, predictable results and higher overall satisfaction.
Choosing a clinic with a strong focus on refractive planning and surgical expertise can make a meaningful difference to accuracy and long-term visual quality.Top of FormBottom of Form
The Role of Technology and Continuous Improvement
Refractive cataract surgery has advanced significantly through ongoing technological innovation. Modern imaging, refined calculation methods, and improved surgical tools have all played a role in enhancing accuracy and consistency. These developments allow surgeons to plan and perform procedures with greater precision than in the past. As technology continues to evolve, outcomes become increasingly reliable.
- Advanced imaging systems – High-resolution diagnostics provide more detailed insight into eye structure and function.
- Refined calculation formulas – Updated lens power formulas improve predictive accuracy across a wider range of eyes.
- Improved surgical tools – Modern instruments enhance control, precision, and safety during surgery.
- Commitment to investment – Clinics that adopt new technology are better positioned to deliver consistent, high-quality results.
- Ongoing refinement of standards – Continuous improvement helps maintain and raise accuracy benchmarks over time.
Understanding this progression helps explain why refractive cataract surgery is more predictable today than ever before. Advances in technology and technique continue to support safer procedures and more precise visual outcomes for patients.
FAQs:
1. How close to perfect vision can I realistically expect after refractive cataract surgery?
Refractive cataract surgery is designed to achieve vision that closely matches your planned visual goal rather than guaranteeing absolute perfection. For most patients, this means vision that is clear, comfortable, and functionally excellent for daily activities such as driving, working, or using digital devices. While many people achieve results very close to their target prescription, small residual variations are normal and usually do not interfere with quality of life. Accuracy should be viewed as achieving meaningful improvement rather than mathematical perfection.
2. Does refractive cataract surgery guarantee freedom from glasses?
Refractive cataract surgery can significantly reduce dependence on glasses, but it does not guarantee complete independence for everyone. Outcomes depend on factors such as lens choice, eye health, and individual visual needs. Some patients may still prefer glasses for specific tasks like prolonged reading or night driving, even when surgery is highly accurate. The key goal is improved visual flexibility and comfort rather than an absolute promise of no spectacles.
3. How do surgeons decide what vision target is best for me?
The vision target is determined through a detailed pre-operative discussion and assessment. Surgeons consider your lifestyle, work requirements, hobbies, and personal preferences alongside clinical measurements. For example, someone who drives frequently may prioritise distance clarity, while another person may prefer better near or intermediate vision. The accuracy of the final result is judged by how closely it meets this agreed target rather than by a single universal standard.
4. Why can vision still vary slightly even with advanced technology?
Despite highly precise measurements and sophisticated planning, the eye is a living tissue that heals uniquely in each person. Small biological variations such as how the lens settles or how the cornea heals can influence final vision. These differences are usually subtle and fall within expected limits. They reflect natural healing responses rather than problems with the surgery itself.
5. How long does it take to know my final visual accuracy after surgery?
Vision often improves quickly after refractive cataract surgery, but final accuracy is not assessed immediately. The eye needs time to heal and stabilise, which typically takes several weeks. During this period, vision may fluctuate slightly. Surgeons usually evaluate final accuracy once healing is complete to ensure measurements reflect stable and reliable vision rather than temporary post-operative changes.
6. If my vision is slightly off target, does that mean the surgery failed?
A small difference from the intended target does not mean the surgery has failed. Minor residual prescriptions are common and often have little impact on daily vision. In many cases, no additional treatment is required, or simple glasses can address specific tasks. The success of surgery is based on overall visual function and satisfaction, not just numerical precision.
7. What role does astigmatism play in vision accuracy after surgery?
Astigmatism can significantly influence visual sharpness if it is not properly addressed. Even with accurate lens power calculations, uncorrected astigmatism can reduce clarity. Modern refractive cataract surgery places strong emphasis on identifying and managing astigmatism through precise measurements and appropriate correction methods. When astigmatism is handled effectively, overall accuracy and visual quality improve substantially.
8. Are enhancement procedures common after refractive cataract surgery?
Enhancements are not routine for most patients. The majority achieve vision that is close enough to their intended target that no refinement is needed. When enhancements are performed, they are usually minor adjustments to fine-tune vision rather than correct major issues. Knowing that refinement options exist can provide reassurance without implying that additional procedures are expected.
9. Does age affect how accurate my vision will be after surgery?
Age does not significantly reduce the accuracy achievable with refractive cataract surgery. Many older patients achieve excellent and stable visual outcomes. What may differ is the speed of recovery, as healing can be slightly slower. Accuracy remains high across age groups, provided the eyes are healthy and surgery is well planned.
10. How important is surgeon experience in achieving accurate results?
Surgeon experience is a key factor in achieving consistent and accurate outcomes. While technology provides detailed data, interpreting those measurements and applying them effectively during surgery requires skill and judgement. Experienced surgeons are better equipped to manage subtle variables, tailor plans to individual needs, and assess healing patterns after surgery. This expertise contributes significantly to both visual accuracy and long-term satisfaction.
Final Thoughts: Understanding Vision Accuracy After Refractive Cataract Surgery
Refractive cataract surgery offers a high level of precision, aiming to align your post-operative vision with the visual goals discussed before surgery. While absolute perfection cannot be guaranteed due to natural healing variations and individual eye factors, modern technology, careful planning, and surgeon expertise make outcomes highly reliable for most patients. Minor differences from the intended target are common, and enhancements are available if needed to fine-tune results.
Ultimately, the success of surgery is measured not only by numerical accuracy but by how well your vision supports daily life distance, near, and intermediate activities comfortably and confidently. Understanding the realistic expectations of vision accuracy can help you approach surgery with confidence and make informed decisions that prioritise both clarity and quality of life. If you are thinking about refractive cataract surgery in London, you can contact us at the London Cataract Centre today.
References:
1. Cooke, D.L., Cooke, T.M. and Myers, R.W., 2022, Limits of the precision in refractive results after cataract surgery, Journal of Cataract & Refractive Surgery, vol. 48, pp. https://www.sciencedirect.com/science/article/abs/pii/S2173579422000767
2. Arens, S., Böhringer, D., Lapp, T., Reinhard, T. and Heinzelmann‑Mink, S., 2024, Comparative analysis of refractive outcomes following cataract surgery using IOL Master 500 and IOL Master 700 biometry devices: a retrospective analysis, Journal of Clinical Medicine. https://www.mdpi.com/2077-0383/13/17/5125
3. Al Barri, L., Mercea, N., Ionela‑Iasmina, Y., Munteanu, M. & Stanca, H.T. (2025) Evaluation of Refractive Predictive Accuracy in Intraocular Lens Power Calculations: A Comparative Study of Swept‑Source Optical Coherence Tomography and Optical Low‑Coherence Interferometry, Journal of Clinical Medicine, 14(4), 1201. https://www.mdpi.com/2077-0383/14/4/1201
4. Refractive Outcomes after Cataract Surgery: Impact of Biometry and Factors Affecting Accuracy (2023) Diagnostics, 12(2), 243. https://pubmed.ncbi.nlm.nih.gov/35204334/ 5. Comparison of Intraocular Lens Formulas in Patients With Postoperative Refractive Surprise (2024) Cureus, 16(12): e74991. https://pubmed.ncbi.nlm.nih.gov/39744283/

