If you have astigmatism and you’re considering cataract surgery or refractive lens exchange, you may be wondering how reliable toric lenses really are. Many people ask whether a toric IOL can fully correct astigmatism, or whether it will only reduce it. You might also wonder why some people end up spectacle free while others need glasses for certain tasks.
In this detailed guide, I want to walk you through everything you need to know about how accurate toric lenses are, how surgeons measure that accuracy, and what affects the final outcome. I’ll also explain what realistic spectacle independence looks like after surgery, and how you can set expectations that match your lifestyle and vision goals.
Understanding Astigmatism: Why It Matters for IOL Accuracy
Astigmatism occurs when the cornea isn’t perfectly spherical. Instead of having a uniform curve, it is shaped more like an oval or a rugby ball, which means light entering the eye is bent unevenly. Because different meridians of the eye focus light at different points, vision can appear blurred, stretched, or distorted at both near and far distances.
Before cataract or lens replacement surgery, astigmatism can come from both the cornea and the eye’s natural lens. Once the natural lens is removed, however, corneal astigmatism becomes the sole remaining source. This makes accurate measurement and correction of the cornea absolutely essential if the goal is sharp vision without dependence on glasses.
How Toric Lenses Are Designed to Correct Astigmatism
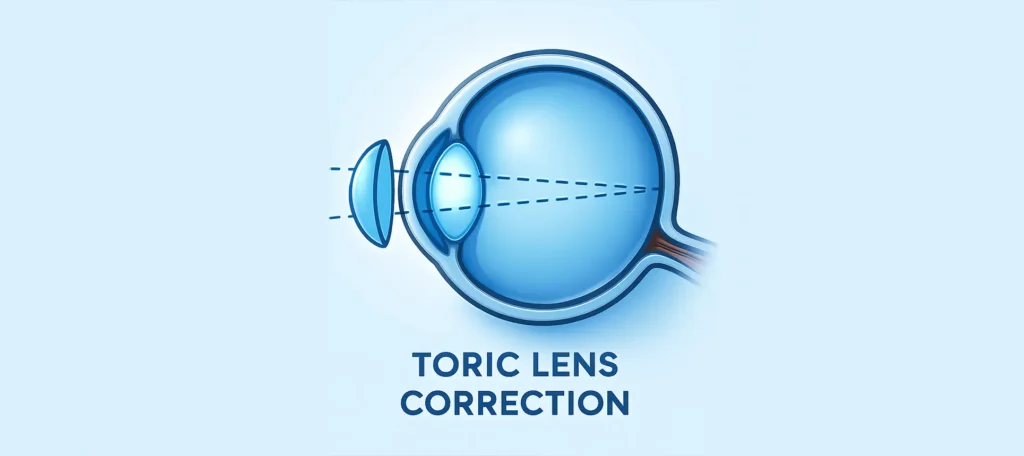
Toric intraocular lenses differ from standard monofocal IOLs because they are not uniform in optical power. Instead, they are engineered with different strengths along specific axes to match the steep and flat meridians of the cornea. When these axes are aligned correctly, the toric lens counteracts the irregular corneal curvature, allowing light to focus more precisely on the retina and producing clearer, sharper vision.
A useful way to understand this is to think of toric glasses. The correction only works when the lenses are positioned at the correct angle if the glasses rotate or tilt, the astigmatism correction fails. The same principle applies inside the eye. A toric IOL must be implanted at a precise orientation and remain stable afterward. Even small degrees of rotation can significantly reduce how effectively the lens corrects astigmatism.
How Surgeons Measure Toric Accuracy
Before a toric lens is selected, your surgeon carries out a detailed pre-operative assessment to ensure the correction is as accurate and predictable as possible. Toric IOL planning is far more involved than simply measuring whether you have astigmatism it requires multiple cross-checked measurements to minimise the risk of error and maximise visual clarity after surgery.
1. Keratometry and Corneal Topography: The most essential data comes from the curvature of your cornea. Surgeons measure this using keratometry and topography devices, which map the shape of your cornea and detect any irregularities.
2. Total Corneal Power (Not Just the Front Surface): Modern systems measure both the front and back surfaces of your cornea. Older systems only measured the front, which sometimes led to under- or over-correction.
3. Axis Verification: The amount of astigmatism alone isn’t enough to ensure accurate correction the exact axis of corneal steepness is just as critical. Even a small rotational error of a few degrees can significantly reduce how well a toric lens works.
4. Biometry Accuracy: Your eye length, anterior chamber depth, and corneal curvature all influence the IOL calculation formulas. Toric IOL calculators integrate these values to determine the exact lens power and orientation.
Understanding how much work goes into selecting your toric lens may reassure you that toric accuracy is not guesswork it’s a precise, multi-step process.
What Level of Correction Can Toric Lenses Achieve?
Most patients understandably want to know whether toric lenses can fully correct their astigmatism. In many cases, they can. Toric IOLs are specifically designed to address regular corneal astigmatism, and for a large proportion of patients, they provide complete or near-complete correction. This often means clear distance vision without the need for glasses for everyday activities such as driving, watching television, or recognising faces.
That said, the level of correction achieved depends on how much astigmatism you have and how your eye heals after surgery. Many patients are left with little to no residual prescription. Others may have a very small remaining astigmatism often less than 0.50 dioptres which is usually subtle and not noticeable in daily life. In these cases, glasses may only be needed for fine tasks or prolonged visual work.
Factors That Influence How Accurate Toric Lenses Are
Even though toric lenses are designed with high precision, their final accuracy can be influenced by several biological and surgical factors. The eye is a living structure, and healing responses vary from person to person. Understanding what can affect toric performance helps set realistic expectations and explains why surgeons place so much emphasis on careful planning, measurement, and follow-up.
1. Lens Rotation After Surgery: Lens rotation after surgery is the most common reason a toric lens may lose accuracy. Even small degrees of rotation can significantly reduce its effectiveness around 17% with a 5-degree shift and about 33% with a 10-degree shift. A rotation of 30 degrees can make the astigmatism correction essentially ineffective
2. Healing and Capsular Contraction: Your lens sits inside a structure called the capsular bag. As the bag heals, it may shrink slightly, influencing the position of the lens. Most of the time, this actually helps stabilise the lens, but in rare cases, it can cause rotation.
3. Corneal Irregularity: Toric lenses work best when astigmatism is “regular,” meaning the two main meridians are symmetrical and predictable. If you have irregular astigmatism from keratoconus, previous eye surgery, or scarring, a toric lens may be less accurate.
4. Incorrect Measurements (Rare but Possible): Measurement errors are uncommon in high-quality clinics, but factors such as dry eye can temporarily distort readings. Treating dryness before biometry improves accuracy.
5. Refractive Surprises: Every eye heals slightly differently. Even with perfect calculations, a small residual prescription may remain. This is typically correctable with glasses, contact lenses, or laser enhancement.
Knowing these variables helps you set realistic expectations and understand why some patients achieve perfect correction while others have small residual errors.
How Toric Lenses Perform for Different Levels of Astigmatism
The way toric lenses perform depends largely on the amount of astigmatism being corrected. In people with low astigmatism, typically between 0.75 and 1.50 dioptres, toric lenses are extremely precise.
For moderate astigmatism, usually in the range of 1.50 to 3.00 dioptres, toric lenses still deliver excellent outcomes. Most patients notice a significant improvement in clarity and visual sharpness, although a small amount of residual astigmatism can sometimes remain.
High astigmatism, above 3.00 dioptres, is more complex to correct. Stronger toric lenses are required, and these are more sensitive to even slight rotation within the eye. While the likelihood of some remaining astigmatism is higher, many patients still experience a major improvement in vision compared with non-toric lenses, particularly in terms of overall clarity and visual comfort.
Astigmatism Correction With Toric Multifocal Lenses

Astigmatism correction with toric multifocal lenses can offer a high level of visual freedom, but it also demands greater precision than monofocal options. These lenses are designed to correct corneal astigmatism while simultaneously addressing presbyopia, allowing clear vision at distance, intermediate, and near. When everything is accurately aligned, patients can enjoy excellent vision across multiple ranges without relying heavily on glasses.
However, toric multifocal lenses are far less forgiving of small residual errors. Even as little as 0.50 dioptres of uncorrected astigmatism can noticeably reduce image quality, leading to blur, glare, or reduced contrast effects that are often more pronounced than with monofocal toric lenses. This sensitivity means that pre-operative measurements, surgical alignment, and post-operative stability all need to be extremely precise.
How Surgeons Improve Toric Lens Accuracy During Surgery
Achieving high accuracy with a toric lens is not just about choosing the right implant it also depends on how precisely it is positioned during surgery. Even small alignment errors can reduce the lens’s effectiveness, so surgeons rely on advanced intraoperative techniques to maximise precision and stability.
1. Digital Alignment Systems: Systems like Callisto, Verion, or ORA generate digital overlays that map the eye’s unique landmarks. These overlays guide the surgeon in positioning the toric lens at the exact planned angle.
2. Intraoperative Aberrometry: Intraoperative aberrometry measures your eye while you are on the operating table. It allows the surgeon to refine lens power selection and confirm the optimal alignment axis in real time.
3. Femtosecond Laser-Assisted Surgery: Femtosecond lasers create highly precise corneal incisions and capsulotomies. This precision helps centre the lens more accurately and improves its long-term stability. Better lens positioning reduces the risk of postoperative rotation.
4. Secure Positioning and Rotation Tests: Before completing the procedure, the surgeon carefully checks that the lens is stable within the capsular bag. The lens may be gently rotated and rechecked to confirm it remains aligned. This step helps ensure lasting accuracy after surgery.
Do Toric Lenses Provide Complete Spectacle Independence?
Toric lenses can significantly reduce your dependence on glasses, but complete spectacle independence is not guaranteed for everyone. Many patients do achieve excellent uncorrected vision, particularly for distance, but the final outcome depends on several individual factors rather than the lens alone.
Your level of independence is influenced by the type of toric lens chosen (monofocal, multifocal, or EDOF), how your eye heals, whether any small residual prescription remains, and your visual demands. Factors such as pupil size, previous prescription strength, and personal expectations also play an important role, especially with multifocal designs that are more sensitive to minor imperfections.
Monofocal toric lenses tend to deliver the sharpest and most stable distance vision with the least risk of glare or halos, though most people still need reading glasses for near tasks. Multifocal toric lenses, on the other hand, can provide vision at multiple distances but require precise correction and a period of adaptation to achieve the best results.
How Surgeons Handle Residual Astigmatism After Surgery

Even with careful planning and precise surgery, a small amount of residual astigmatism can sometimes remain after toric lens implantation. In many cases, this residual astigmatism is very minor and may not noticeably affect vision, meaning no further intervention is necessary.
For those who do notice visual disturbances, there are several non-invasive options to manage residual astigmatism. Prescription glasses can correct minor refractive errors for specific tasks, such as reading or night driving.
In certain cases where residual astigmatism is caused by lens rotation or misalignment, the surgeon may reposition the toric lens to restore accuracy. Rarely, if these measures aren’t sufficient, a lens exchange might be considered.
Why Your Surgeon May Recommend a Toric Lens Even for Mild Astigmatism
Even mild astigmatism can subtly blur vision, particularly in low-light conditions or when performing tasks that require fine detail, such as reading, computer work, or driving at night. This small refractive error may seem insignificant during the day but can become noticeable in dim light or when contrast is low.
By choosing a toric lens, patients can achieve sharper, more precise vision across all distances and lighting conditions. This not only improves visual comfort but also reduces dependence on corrective glasses for everyday activities. Even astigmatism as low as 0.75 dioptres can make a meaningful difference in clarity when corrected with a toric IOL.
For these reasons, many surgeons now recommend toric lenses proactively, ensuring patients experience the clearest possible vision post-surgery. Correcting even mild astigmatism can enhance overall quality of vision and minimize visual disturbances like glare or halos.
Common Myths About Toric IOL Accuracy
Toric IOLs are a highly effective solution for correcting astigmatism, but misconceptions can create unnecessary hesitation for patients. Many people worry about rotation, incomplete correction, or increased visual disturbances, even though modern toric lenses are designed for stability and precision.
1. Myth: Toric lenses often rotate: Modern toric IOLs are designed with features that help them stay stable within the eye’s capsular bag. Rotation is uncommon, and surgeons check alignment carefully during surgery to ensure lasting stability. If rotation does occur, it is usually minor and correctable.
2. Myth: Toric lenses can’t fully correct astigmatism: Toric lenses are specifically designed to correct astigmatism, particularly when it is regular in shape. Most patients achieve a significant reduction in astigmatic blur. For complex cases, surgeons may combine toric IOLs with other techniques for optimal results.
3. Myth: Toric lenses cause more glare or halos: Monofocal toric lenses function like standard monofocal lenses, so they do not inherently increase glare or halos. Visual disturbances are more often related to individual healing or pre-existing eye conditions. Proper lens selection helps minimise any potential side effects.
4. Myth: Toric IOLs are only for high astigmatism: Even low levels of astigmatism can impact vision, particularly for distance clarity. Toric lenses can correct mild to moderate astigmatism, improving overall sharpness and reducing dependence on glasses.
How Age and Eye Anatomy Influence Toric Accuracy
The accuracy of toric lenses doesn’t depend solely on the lens itself; your individual eye anatomy plays a crucial role. Factors such as the overall shape of your eye, corneal curvature, and internal structures can influence how well the lens performs. Patients with unusually long or short eyes may experience slightly more variability in outcomes, and conditions like keratoconus or corneas that have undergone previous LASIK surgery require careful preoperative planning.
Age can also have an impact. Older patients may experience more capsular contraction during healing, which can subtly affect lens orientation. However, modern toric IOLs are specifically designed to minimise rotation and maintain stability, even in these cases.
During your consultation, your surgeon will thoroughly assess these anatomical factors, ensuring that the chosen toric lens and surgical plan are tailored to provide the best possible visual outcome.
Why Toric Lenses Are More Accurate Today Than Ever Before
Toric lenses have become far more accurate today than in the past. Decades ago, outcomes were less predictable, and patients sometimes experienced rotation or residual astigmatism. Advances in lens materials and more stable haptics have greatly improved the physical stability of the lenses inside the eye.
In addition, modern digital surgical guidance, precise corneal mapping, improved IOL calculation formulas, and real-time intraoperative measurements allow surgeons to plan and place toric lenses with remarkable precision. These innovations mean that today’s toric lenses can achieve visual results that were virtually impossible just a generation ago.
Setting Realistic Expectations for Your Vision After Toric IOLs
Toric lenses offer excellent accuracy, but it’s important to remember that no technology can guarantee perfect vision. While most patients achieve significant improvements, a realistic perspective helps manage expectations.
You can expect clearer distance vision and a substantial reduction or even full correction of your astigmatism. This often translates into sharper, more comfortable vision, especially for daily activities.
However, you may still need reading glasses, particularly if you choose monofocal toric lenses. Understanding these likely outcomes allows you to feel confident and comfortable with your decision, knowing the benefits and limitations of the procedure.
When Toric Lenses Are NOT the Right Choice
Toric lenses are highly effective for many patients, but they aren’t suitable for everyone. If you have irregular astigmatism, an unstable cornea, or advanced keratoconus, a toric lens may not provide the desired correction or could lead to suboptimal results. Similarly, if your lens capsule is unstable, the lens may rotate or shift, reducing its effectiveness.
In addition, patients with inconsistent or unreliable measurements during preoperative assessment may not achieve predictable outcomes with a toric lens. In such situations, your surgeon may recommend alternative solutions, such as monofocal lenses with glasses correction or other vision-correcting strategies, to ensure the best possible visual results.
FAQs:
1. Can toric lenses fully correct astigmatism?
Toric lenses are specifically designed to address regular corneal astigmatism, and in many patients, they can provide complete or near-complete correction. The level of correction depends on the severity of your astigmatism, the accuracy of preoperative measurements, and the stability of the lens after implantation.
2. How do surgeons ensure toric lens accuracy?
Surgeons use a combination of advanced measurements and imaging technologies to maximise toric lens accuracy. Corneal topography and keratometry assess the precise curvature of the cornea, while total corneal power measurements account for both the front and back surfaces. Axis verification ensures the toric lens is aligned with the steep meridian of the cornea.
3. What factors can affect the performance of toric lenses?
Several biological and surgical factors influence toric lens performance. Lens rotation after surgery is the most common cause of reduced accuracy, and even small degrees of rotation can impact visual outcomes. Healing patterns and capsular contraction may subtly alter lens orientation, while irregular corneal shapes, previous eye surgery, or scarring can reduce effectiveness.
4. How do toric lenses perform for different levels of astigmatism?
Toric lenses are highly effective for low to moderate astigmatism, typically ranging from 0.75 to 3.00 dioptres, with many patients achieving excellent distance vision and minimal residual prescription. In patients with high astigmatism above 3.00 dioptres, toric lenses still provide substantial improvement, although outcomes are more sensitive to lens rotation or alignment.
5. Can toric multifocal lenses provide astigmatism correction across all distances?
Toric multifocal lenses combine correction for astigmatism with presbyopia management, providing vision at distance, intermediate, and near. They require precise measurements and careful alignment, as even small residual astigmatism can reduce image quality and contrast. When accurately implanted, these lenses can offer excellent visual freedom and reduced dependence on glasses.
6. Will I achieve complete spectacle independence with a toric lens?
Toric lenses can greatly reduce the need for glasses, particularly for distance vision. Monofocal toric lenses provide stable and sharp distance clarity, although reading glasses may still be necessary for near tasks. Multifocal toric lenses can offer vision at multiple distances but require precise alignment and adaptation. The final level of spectacle independence depends on individual eye anatomy, healing patterns, and the type of toric lens chosen, making consultation with a skilled surgeon essential to match expectations with realistic outcomes.
7. What happens if residual astigmatism remains after surgery?
Minor residual astigmatism is not uncommon and often does not significantly affect daily vision. If visual disturbances persist, they can be addressed through non-invasive measures such as glasses for specific tasks or laser vision correction procedures like LASIK or PRK. In rare cases where residual astigmatism results from lens rotation, a surgeon may reposition the toric lens. Very few patients require a complete lens exchange.
8. Are toric lenses suitable even for mild astigmatism?
Even mild astigmatism can cause noticeable blur or reduced visual clarity, particularly in low-light or high-contrast situations. Correcting small amounts of astigmatism with a toric lens can improve overall visual comfort and distance clarity, reduce reliance on glasses, and minimize visual disturbances such as glare. Many surgeons now recommend toric lenses proactively, even for mild astigmatism, to provide the sharpest possible vision after cataract or lens replacement surgery.
9. How does age or eye anatomy affect toric lens accuracy?
Eye anatomy and age can influence toric lens outcomes. Variations in eye length, corneal shape, or internal structures may slightly affect lens positioning and visual clarity. Older patients may experience greater capsular contraction during healing, which could influence lens orientation, though modern toric lenses are designed to maintain stability.
10. Why are modern toric lenses more accurate than earlier versions?
Advances in lens design, materials, and surgical techniques have significantly improved toric lens accuracy. Modern lenses feature more stable haptics that reduce rotation, and digital surgical guidance allows precise alignment. Improved corneal mapping, refined IOL calculation formulas, and intraoperative aberrometry enable real-time adjustments, resulting in outcomes that were far less predictable in the past.
Final Thought: Achieving Clearer Vision with Toric Lenses
Toric lenses are a highly effective option for correcting astigmatism, offering clearer vision and reducing reliance on glasses for many patients. While results depend on factors like corneal shape, lens alignment, and individual healing patterns, modern toric IOLs provide remarkable precision and stability. If you’re considering toric lenses in London, you can reach out to us at London Cataract Centre to discuss whether this treatment is the right choice for your vision goals.
References:
1. Li ES, Vanderford EK, Xu Y, Kang PC. Rotational stability of toric intraocular lenses by lens model and haptic design: systematic review and single‑arm meta‑analysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC11338026/
2. Toric intraocular lens: a literature review. Postoperative residual refractive astigmatism and visual outcomes with toric IOLs. https://pmc.ncbi.nlm.nih.gov/articles/PMC11254006/
3. Rotational stability of Toric intraocular lenses. Rotational stability and visual outcomes with toric IOLs. https://www.sciencedirect.com/science/article/abs/pii/S0377123720300526
4. Nemet AY, Reitblat O, Levy A, Nemet E, Assia EI. Clinical outcomes following toric intraocular lens implantation: Case series study. https://www.mdpi.com/2077-0383/14/7/2316
5. Park RB. Astigmatism management in modern cataract surgery. https://www.mdpi.com/2411-5150/8/1/9

