Cataract surgery has become one of the safest and most successful operations in modern medicine, with millions of people worldwide regaining clear vision every year. But even with such excellent outcomes, surgeons are always looking for ways to make the procedure even safer. One of the areas attracting growing attention is the role of heat in phacoemulsification – the most common cataract surgery technique.
During phacoemulsification, ultrasound energy is used to break up the cloudy lens so it can be removed and replaced with an artificial intraocular lens (IOL). While this process is highly effective, it does generate heat at the tip of the ultrasound probe. If temperatures rise too high, even for a short time, there’s a risk of thermal injury to the cornea or incision site.
That’s where thermal imaging, particularly infrared cameras, comes into the picture. By monitoring real-time temperature changes inside the eye or around surgical instruments, researchers hope to improve safety, avoid corneal burns, and optimise the energy settings used during surgery. In this article, we’ll explore what thermal imaging is, why it matters in cataract surgery, what the latest research shows, and whether you as a patient might one day benefit from this emerging technology.
Understanding Heat in Cataract Surgery
When surgeons perform phacoemulsification, they insert a thin probe into the eye through a small incision. The probe vibrates at ultrasonic speeds to emulsify the cataract so that it can be aspirated out. This process inevitably generates friction and heat, especially at the incision site where the probe passes through.
Normally, surgeons use balanced salt solution (BSS) irrigation and specific probe sleeve designs to keep the temperature under control. But despite these precautions, there is still a small risk of localised heating that could cause damage. Corneal burns, while rare, are well-documented complications that can lead to scarring, irregular astigmatism, and a more difficult recovery.
The problem is that heat build-up is invisible to the naked eye during surgery. A surgeon can’t directly see temperature changes, and by the time tissue damage is noticed, it may already be too late. This is where thermal imaging technology offers a potentially game-changing solution – providing a window into something surgeons have always had to guess or infer indirectly.
What Is Thermal Imaging?
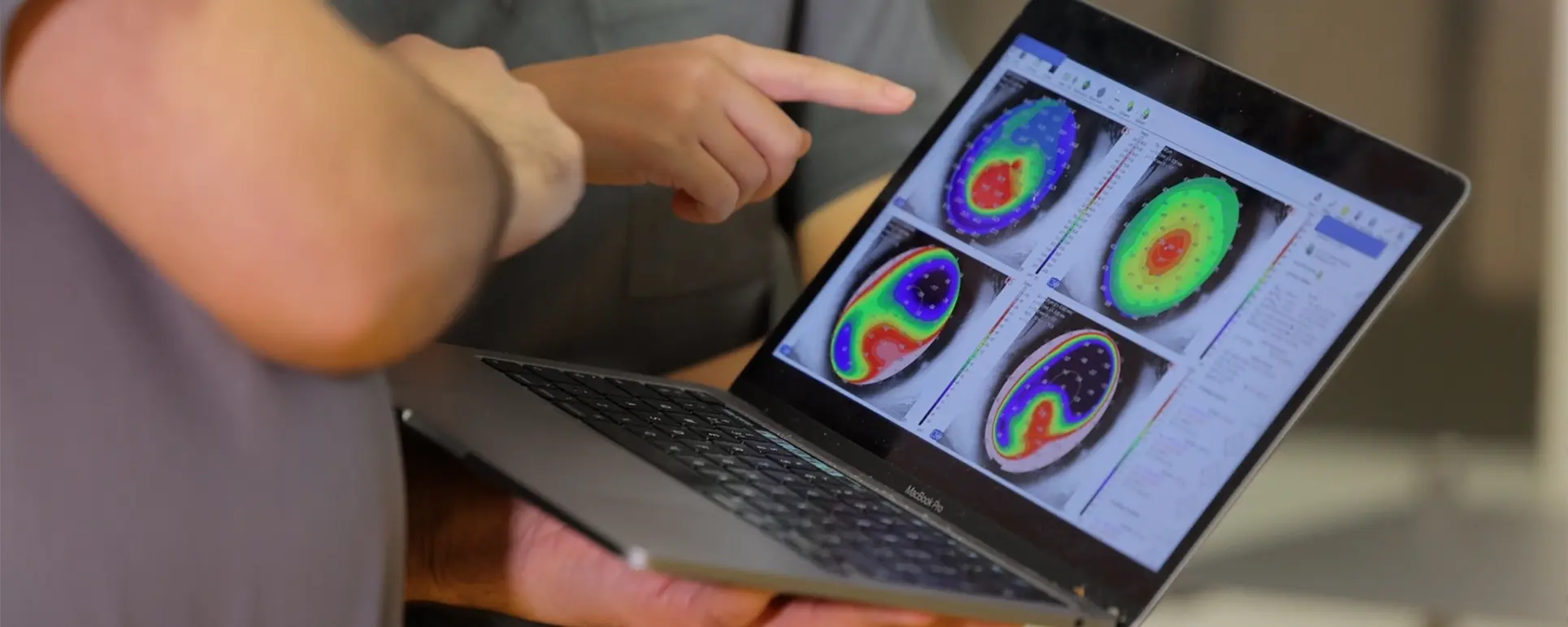
Thermal imaging, sometimes called infrared imaging, is a way of detecting and visualising heat. Infrared cameras pick up the radiation emitted by objects based on their temperature and convert it into a visual map, usually displayed as colours. Warmer areas appear as brighter or hotter colours, while cooler areas show as darker shades.
Outside of medicine, you’ve probably seen thermal imaging in action in areas like building inspections, wildlife documentaries, or even airport security. But in healthcare, its applications are steadily expanding. From detecting fevers to mapping blood flow, infrared imaging provides a non-invasive way to monitor subtle physiological changes.
In the context of cataract surgery, the idea is to use compact infrared sensors or cameras to watch the surgical field in real time. This could give surgeons a precise indication of whether heat is building up around the probe or corneal incision, allowing them to make immediate adjustments before damage occurs.
Why Heat Monitoring Matters

You might wonder why such attention is paid to a relatively rare complication like corneal burns. The answer lies in both safety and efficiency.
First, even though corneal burns don’t happen often, when they do occur they can be very problematic. Patients may require additional treatment, may experience worse visual outcomes, and in some cases may even need corneal transplantation. Preventing even a handful of these cases is a major benefit.
Second, monitoring heat could help surgeons fine-tune their use of ultrasound energy. Phacoemulsification machines already come with sophisticated settings to adjust pulse duration, duty cycle, and energy levels. Real-time temperature feedback could help surgeons use the minimum energy necessary, leading to less trauma to the eye overall and faster recovery for the patient.
Third, there’s a broader interest in surgical sustainability. Using less energy not only benefits the patient but also aligns with efforts to make medical procedures more efficient and environmentally responsible. By identifying ways to reduce unnecessary heat and power usage, thermal imaging may play a role in this bigger picture.
How Infrared Cameras Could Be Integrated
The practical question is: how exactly would an infrared camera or thermal sensor work in the setting of cataract surgery? Researchers are exploring several approaches.
One option is to mount a small thermal camera onto the operating microscope. This would allow the surgeon to see both the visible surgical field and an overlay of temperature data. Another idea is to integrate micro-sensors into the phacoemulsification probe or sleeve itself, so that readings are taken as close as possible to the source of heat.
There are also discussions about using external devices placed near the surgical field to monitor overall heat patterns. Each of these methods has advantages and challenges, from cost and complexity to ensuring that the equipment doesn’t interfere with the delicate manoeuvres of eye surgery.
What the Research Shows So Far
Studies have already been conducted in laboratory and simulated settings. For example, researchers have used infrared cameras to record the heat generated during phacoemulsification at different energy levels and with different probe designs. These experiments show clear differences in how much heat builds up depending on the surgical settings and irrigation flow.
Some early work suggests that with real-time thermal monitoring, it’s possible to spot rising temperatures before they reach harmful levels. This means a surgeon could reduce ultrasound power, adjust fluidics, or pause briefly to allow cooling – all before any damage occurs.
Clinical studies in actual patients are more limited, but the concept is gaining traction. Conferences in ophthalmology now include discussions about integrating thermal imaging, and technology companies are exploring compact, surgical-grade sensors that could be adapted for routine use.
Benefits for Patients

From a patient’s perspective, the most obvious benefit of thermal imaging in cataract surgery is added safety. Knowing that your surgeon has an extra tool to prevent rare but serious complications like corneal burns can be very reassuring.
There may also be indirect benefits. If surgeons can use less energy while still breaking up the cataract effectively, this could mean less inflammation inside the eye, a smoother healing process, and possibly clearer vision sooner after the operation.
Another potential advantage is that by gathering data from thousands of surgeries, doctors could refine best practices for different cataract types and patient profiles. Over time, this could make outcomes even more predictable and tailored to individual needs.
Challenges and Limitations
Of course, no new technology is without hurdles. There are practical challenges in making thermal imaging work seamlessly in the operating theatre.
First, the eye is a small and delicate organ. Adding sensors or overlays must not distract the surgeon or clutter the already complex surgical view. The equipment needs to be lightweight, unobtrusive, and easy to interpret.
Second, the cost of implementing such systems could be a barrier, at least initially. High-quality medical-grade thermal cameras are not cheap, and hospitals will need to weigh the benefits against other priorities.
Third, there’s the issue of data interpretation. Heat patterns in the eye may vary depending on irrigation flow, surgical technique, and patient anatomy. Surgeons will need training and clear guidelines to know how to respond to the information without overreacting or slowing down unnecessarily.
Future Directions
Looking ahead, thermal imaging may not just be about preventing corneal burns. It could also provide insights into other aspects of cataract surgery. For example, by monitoring how heat dissipates, researchers may learn more about fluid dynamics in the anterior chamber.
There is also the possibility of integrating artificial intelligence (AI). AI systems could analyse the thermal data in real time and alert the surgeon only if a dangerous threshold is approached, avoiding information overload. This kind of “smart assistant” could make the technology more practical in daily use.
Finally, thermal imaging might one day be combined with other intraoperative imaging modalities such as optical coherence tomography (OCT). Together, they could provide a more complete picture of what’s happening inside the eye – from structure to temperature – making cataract surgery safer and more personalised than ever.
FAQ: Thermal Imaging and Cataract Surgery
1. What is the main risk thermal imaging aims to prevent in cataract surgery?
The biggest risk that thermal imaging seeks to reduce is corneal burns, which are caused by excess heat from the phacoemulsification probe during cataract surgery. While these burns are rare, they can lead to corneal scarring, delayed healing, and even poorer visual outcomes. By giving surgeons real-time insight into temperature changes, thermal imaging allows them to act early and prevent damage before it happens.
2. How do infrared cameras detect heat during surgery?
Infrared cameras detect the natural radiation given off by objects according to their temperature. In cataract surgery, the camera can pick up the heat emitted from the surgical instruments or tissues and translate this into a visual display of colours or numbers. This allows the surgeon to see precisely where heat is building up in the surgical field, making it easier to adjust energy use and fluidics on the spot.
3. Has thermal imaging already been used in live cataract surgeries?
So far, thermal imaging has mainly been studied in laboratory and experimental models, where it has successfully shown how heat builds up under different surgical conditions. There have also been small pilot trials in real cataract surgeries, but the technology is not yet part of routine practice. It is still being refined to ensure it works reliably in the fast-moving environment of the operating theatre.
4. Will patients notice any difference if thermal imaging is used?
Patients won’t notice any change during the procedure itself, since the infrared cameras or sensors are used entirely by the surgical team. What they may experience, however, is greater safety and possibly quicker recovery afterwards if thermal imaging helps the surgeon minimise energy use and reduce unnecessary tissue trauma. From the patient’s perspective, the procedure will feel no different.
5. Does using thermal imaging increase the cost of cataract surgery?
At the moment, thermal imaging is still in development, and introducing it into operating theatres would come with extra costs for equipment and training. Whether this would be passed on to patients is uncertain, as much depends on how widely adopted it becomes and whether insurers or health services choose to cover it. Over time, as the technology becomes more common, costs are likely to fall.
6. Can thermal imaging make cataract surgery faster?
The main aim of thermal imaging is to improve safety, but in some cases it may indirectly help surgery run more smoothly. By providing surgeons with immediate feedback on energy use and heat levels, they can make more efficient adjustments without needing to pause and guess. This could make the procedure more predictable and reduce unnecessary delays, though speed is a secondary benefit.
7. Are there any risks to the eye from using infrared cameras?
Infrared cameras are completely safe for patients because they don’t send any radiation into the eye. They work passively by detecting heat that is already being emitted, so there is no extra exposure or risk involved. This means patients can benefit from the added safety of temperature monitoring without having to worry about any side effects from the imaging itself.
8. Could AI be combined with thermal imaging in cataract surgery?
Yes, AI could play a major role in making thermal imaging more practical. Instead of the surgeon having to constantly monitor thermal maps, an AI system could analyse the data in real time and only give alerts when temperatures are approaching dangerous levels. This would make the process more efficient, reduce distractions, and provide an extra layer of reassurance for both surgeon and patient.
9. Is thermal imaging likely to replace other monitoring methods in surgery?
It’s unlikely that thermal imaging would replace existing safeguards, since surgeons already rely on fluidics, probe design, and energy settings to manage heat. Instead, it would complement these measures by providing direct evidence of what’s happening in the eye. This combination of current techniques plus thermal monitoring could together create a much safer surgical environment.
10. When might we see thermal imaging become standard in cataract surgery?
It is still too early to say exactly when thermal imaging will be widely adopted, as the technology needs more clinical trials and refinement. If results continue to be promising, it could start appearing in specialist centres within the next few years, with broader uptake after that. For now, patients should know that it represents an exciting innovation that is steadily moving closer to real-world use.
Final Thoughts
Cataract surgery is already one of the most successful procedures in medicine, but innovation never stops. Thermal imaging is a fascinating development because it tackles a subtle but important aspect of safety: the invisible heat generated by ultrasound.
While still in the research and early clinical trial stage, the idea of using infrared cameras to watch over the surgical field could one day become standard practice. For patients, this means the reassurance that every possible step is being taken to safeguard their eyes and deliver the best outcomes.
At London Cataract Centre, we stay at the forefront of these innovations. Our mission is not only to restore clear vision but also to make sure every operation is performed with the highest possible safety standards. As new technologies like thermal imaging evolve, we’ll continue to evaluate them carefully and adopt those that bring real benefits to our patients.
References
- Giglio, R. (2024) ‘Phacoemulsification wound burn and its management’, Journal of Ophthalmic Surgery, 58, pp. 112-118. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11001284/
- Modrzejewska, A., Cieszyński, Ł., Zaborski, D. and Parafiniuk, M. (2020) ‘Infrared thermography for the analysis of ocular surface temperature after phacoemulsification’, Arquivos Brasileiros de Oftalmologia, 83, pp. 202-208. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11826646/
- Nair, S. (2017) ‘Wound and surface temperatures in vivo in torsional phacoemulsification’, Clinical Ophthalmology, 11, pp. 1234-1241. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5291324/
- Gulias-Cañizo, R., Rodríguez-Malagón, M. E., Botello-González, L., Belden-Reyes, V., Amparo, F. and Garza-León, M. (2023) ‘Applications of infrared thermography in ophthalmology’, Life, 13(3), Article 723. DOI:10.3390/life13030723. Available at: https://doi.org/10.3390/life13030723
- Bissen-Miyajima, H. (1999) ‘Thermal effect on corneal incisions with different phacoemulsification ultrasound tips’, Journal of Cataract & Refractive Surgery, 25(9), pp. 1213-1219.