If you’re planning cataract surgery — or you’re a surgeon helping patients make informed choices — you might be surprised at just how much impact the smallest of decisions can have. One such decision? The location of the incision. While it might seem like a minor technicality, whether the surgeon chooses a temporal (side) or superior (top) incision can have ripple effects on the outcome — not just in the short term but months or even years down the line.
In this article, we’re going to unpack the evidence, look at what the research says, and explain in simple terms how incision location may affect postoperative astigmatism, wound stability, and lens centration. So whether you’re a curious patient or a surgeon wanting to review the evidence, let’s dive into it.
Why Incision Location Matters More Than You Might Think
The main goal of cataract surgery is simple: remove the cloudy natural lens and replace it with a clear intraocular lens (IOL). The route the surgeon takes to get there, though, can make a difference. That route starts with an incision — and that incision has to be safe, stable, and as astigmatism-neutral as possible.
There are a few key incision placements used globally:
- Temporal incision – on the outer (lateral) side of the cornea
- Superior incision – made at the top (12 o’clock) of the cornea
- Oblique incisions – placed between these two points, often superotemporal or superonasal
While they all access the same internal anatomy, they differ in their interaction with the cornea’s natural curvature, lid pressure, gravity, and even exposure to bacteria. Over time, these subtle differences can affect vision clarity and patient satisfaction.
Astigmatism: How Incision Site Shapes the Cornea
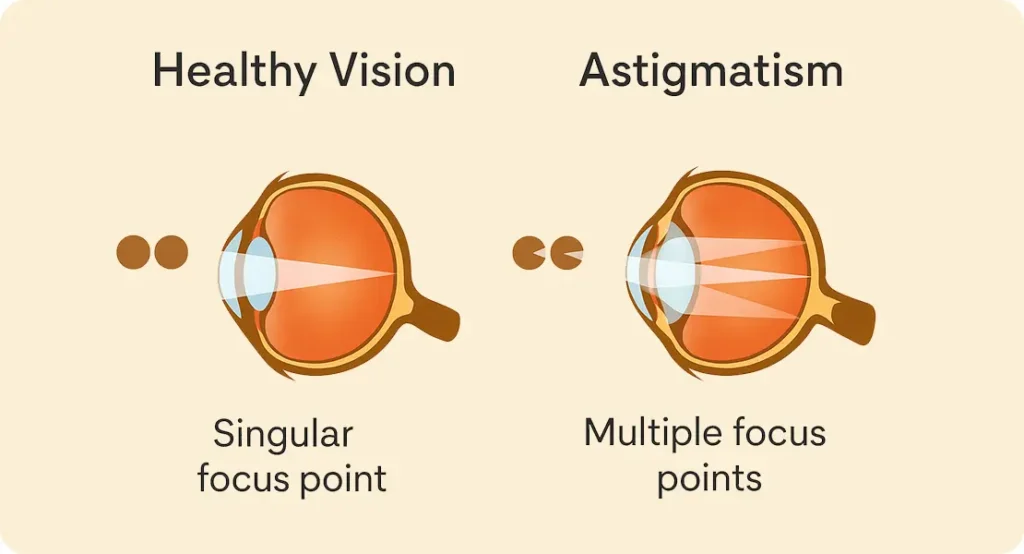
Astigmatism occurs when the cornea is shaped more like a rugby ball than a football — meaning light doesn’t focus evenly on the retina. Even small changes in corneal curvature due to surgical incisions can induce or reduce astigmatism. So the choice of incision site directly affects this outcome.
What the Research Shows
Numerous studies have shown that temporal incisions tend to induce less surgically induced astigmatism (SIA) than superior incisions. One of the reasons is biomechanical — the temporal cornea is less curved than the vertical meridian in most people, so incising here causes less disruption to the overall shape.
For example, a meta-analysis by Altan-Yaycioglu et al. (2007) found that the mean SIA was significantly lower in temporal incisions (around 0.42D) than superior incisions (0.66D). This might not sound like much, but when you’re aiming for precise refractive outcomes — especially in premium IOL cases — every dioptre matters.
Why Temporal Often Wins
The other advantage of temporal incisions is that they align more closely with the natural astigmatic axis in many patients. With-the-rule (WTR) astigmatism, where the vertical meridian is steeper, is more common in younger individuals, while against-the-rule (ATR) astigmatism becomes more prevalent with age — especially in cataract-aged populations. A temporal incision, which flattens the horizontal axis, can therefore partially correct ATR astigmatism.
So, for older patients — the typical cataract demographic — temporal incisions might even offer a minor refractive bonus.
Wound Healing and Stability: Do Some Incisions Heal Better?
Once the lens is in, the surgery is only halfway done. The healing process that follows is crucial — and wound integrity plays a central role in how well the eye recovers and how stable the vision remains.
The Influence of Lid Pressure
One often overlooked factor is eyelid pressure. A superior incision sits right under the upper eyelid. Every time the patient blinks or squeezes their eyes, pressure is applied directly onto the wound. Over time, this could slightly affect how the wound remodels or closes — potentially increasing the risk of induced astigmatism, leakage, or even wound dehiscence in high-risk eyes.
Temporal incisions, by contrast, are off to the side, where they face less direct pressure from blinking. This can result in more predictable wound healing and a lower risk of mechanically induced distortion.
Microbial Access and Infection Risk
Interestingly, the site of the incision may also influence the risk of postoperative infection. Some studies suggest that superior incisions are more exposed to tear pooling under the upper eyelid, which may harbour more bacteria. This is a potential risk factor for endophthalmitis — although the incidence remains low in modern cataract surgery with proper sterile technique.
Temporal incisions, while more exposed to the environment, benefit from better visibility during surgery (especially under topical anaesthesia) and possibly less microbial pooling post-op. The jury is still out on whether one site is definitively safer than the other, but wound architecture and sealing seem to be more consistently stable with temporal approaches.
Centration of the IOL: Could the Incision Shift the Lens?

When an intraocular lens is placed inside the eye, it needs to stay centred to give optimal vision — especially with toric or multifocal lenses. But could the incision location subtly affect IOL positioning?
The Evidence So Far
There’s emerging evidence that superior incisions may create slightly more vertical pressure and torque on the globe, which in some cases can lead to IOL tilt or decentration. This is especially relevant when using lenses that are sensitive to position — like multifocal or toric IOLs.
A study by Bhandari et al. (2013) used anterior segment optical coherence tomography (AS-OCT) to compare IOL tilt and decentration in superior vs temporal incisions. They found that IOLs were more likely to remain centrally aligned with temporal incisions, especially in eyes with pre-existing zonular weakness.
Implications for Premium IOLs
If you’re a patient opting for a premium lens — particularly a multifocal — precise centration is essential. Even a slight decentration of a multifocal IOL can lead to reduced contrast sensitivity, glare, or haloes. So in these cases, a temporal incision might offer a small but meaningful advantage.
Surgeon Ergonomics and Visualisation: A Hidden Factor
Surgeons are people too — and their comfort and posture during surgery can influence the outcome. Many right-handed surgeons prefer temporal incisions on the right eye and superior or superotemporal on the left. This is partly habit and partly due to how they position themselves relative to the microscope.
But there’s more to it. Temporal incisions often offer better exposure and visibility during surgery — especially in deep-set eyes or when operating under topical anaesthesia, where lid retraction is minimal. This can improve safety and speed.
On the other hand, in patients with poor cooperation or severe eye rotation, a superior approach may offer better control. So the “best” incision is sometimes a matter of what allows the surgeon to operate most safely and confidently.
Astigmatic Considerations in Left vs Right Eyes
It’s also worth noting that most surgeons will perform a temporal incision on each eye — which places the incision at 9 o’clock in the right eye and 3 o’clock in the left. This can sometimes lead to asymmetrical astigmatism if the patient’s baseline corneal curvature differs between eyes.
In such cases, the surgeon may opt to individualise incision placement based on the axis of astigmatism, aiming for the most neutral or corrective outcome possible. Some even use intraoperative aberrometry to fine-tune this in real-time.
Are There Patients Better Suited to a Particular Approach?
Yes, absolutely. Incision location should never be one-size-fits-all. Several patient-specific factors can influence the best choice:
- Pre-existing astigmatism – Temporal incisions may help correct ATR astigmatism.
- Deep-set eyes or narrow palpebral fissures – May benefit from temporal approaches for better access.
- Head posture or scoliosis – Sometimes favour superior incisions to allow for better ergonomics.
- Zonular instability or pseudoexfoliation – Might benefit from the more stable centration seen with temporal access.
The key here is customisation. Rather than sticking to one approach for all, many modern surgeons now tailor their incision site to the patient’s anatomy and refractive goals.
The Role of Modern Tools: Imaging and Planning

Thanks to high-resolution corneal topography, optical biometry, and AS-OCT, we can now visualise and simulate the effects of different incision sites before ever making a cut.
These tools allow surgeons to:
- Predict surgically induced astigmatism (SIA)
- Plan incisions to correct or neutralise astigmatism
- Assess potential IOL decentration risk
- Adjust for posterior corneal astigmatism
So while surgical skill is still paramount, technology helps guide incision choices in ways that weren’t possible a decade ago.
Is There a “Best” Incision Location?
In truth, there is no universal “best” — only what’s best for a particular patient, eye, and surgical situation. That said, the literature increasingly leans towards temporal incisions as the more stable, predictable, and astigmatism-neutral option for the majority of patients.
But there are exceptions — and experienced surgeons often develop the skill to operate confidently from multiple angles. Ultimately, the incision is just one piece of a complex surgical puzzle.
Frequently Asked Questions
- Why does incision location matter in cataract surgery?
The position of the incision can subtly influence the shape of your cornea after surgery, which affects astigmatism, wound healing, and how well the new lens sits in the eye. While all incision sites aim to safely access the lens, some offer better visual outcomes or faster healing depending on the individual eye anatomy. - Is a temporal incision better than a superior incision?
For many patients, yes — especially older adults. Temporal incisions tend to induce less astigmatism, heal more predictably, and allow for better IOL centration. However, the best incision site can vary based on the surgeon’s technique, your eye shape, and any pre-existing conditions. - Can the incision location affect how quickly I recover?
Potentially, yes. Temporal incisions are generally away from the upper eyelid, so they face less blinking pressure, which can help with smoother wound healing. Superior incisions, under the upper lid, may take slightly longer to stabilise, though most patients heal well either way with proper care. - Does incision location matter if I’m getting a toric or multifocal lens?
Absolutely. These premium lenses are sensitive to alignment. A well-centred lens is key to optimal vision, and temporal incisions have been shown in some studies to reduce the chance of IOL tilt or decentration, especially in eyes with zonular weakness or asymmetry. - Is it possible to customise the incision location for each eye?
Yes — and many modern surgeons do just that. Depending on your corneal curvature, astigmatism type, or eye anatomy, they may choose different incision sites for each eye to optimise the results. Tools like corneal topography and intraoperative aberrometry can help guide these decisions. - Is one incision site safer than another in terms of infection?
Infection risk is extremely low with modern cataract surgery, but some studies suggest temporal incisions might carry a slightly lower risk due to better exposure and wound visibility. That said, sterile technique and post-op hygiene are far more important than location alone. - Can incision site be changed during surgery?
In theory, yes, but in practice surgeons plan incision sites before surgery based on your pre-op measurements. In rare cases where unexpected challenges arise, they may adjust the incision intraoperatively, but that’s typically only done by highly experienced surgeons. - Should I ask my surgeon which incision they’ll use?
It’s a good idea, especially if you’re having premium lenses implanted or want to understand your astigmatism correction plan. Most surgeons are happy to explain their approach and reassure you that their chosen method is tailored to your eyes.
Final Thoughts: Small Decisions, Big Differences
It’s easy to underestimate the role that a few millimetres of incision placement can have on something as complex and critical as your vision. But as we’ve seen, the evidence is building — and that evidence suggests that temporal incisions, in general, offer a subtle but measurable edge in terms of astigmatism control, wound healing, and IOL centration.
So, if you’re a patient preparing for cataract surgery, don’t be afraid to ask your surgeon about their approach. And if you’re a surgeon, it’s worth reflecting on whether adapting incision sites to each eye’s unique anatomy could push your outcomes even further.
References
- Altan‑Yaycioğlu, R., Akova, Y. A., Akça, S. & Gültekin, S., 2007. Effect on astigmatism of the location of clear corneal incision in phacoemulsification. Journal of Cataract & Refractive Surgery, 33(4), pp.508–512. Available at: https://pubmed.ncbi.nlm.nih.gov/17523515/ (Accessed July 2025)
- Roman, S., Givort, G. & Ullern, M., 1997. Choice of the site of incision for cataract surgery without suture according to preoperative astigmatism. Journal Français d’Ophtalmologie, 20(9), pp.673–679. French language, see PMID: 9587578 (pubmed.ncbi.nlm.nih.gov)
- Rho, C. R. & Joo, C. K., 2012. Effects of steep meridian incision on corneal astigmatism in phacoemulsification cataract surgery. Journal of Cataract & Refractive Surgery, 38(4), pp.666–671. ResearchGate summary (Accessed July 2025)
- Ashena, Z., Maqsood, S., Ahmed, S.N. & Nanavaty, M.A., 2020. Effect of intraocular lens tilt and decentration on visual acuity, dysphotopsia and wavefront aberrations. Vision, 4(3), p.41. Available at: https://www.mdpi.com/2411-5150/4/3/41 (Accessed July 2025)
- Journal of the Canadian Journal of Ophthalmology, 2007. Astigmatism induced by oblique clear corneal incision: right vs left eyes (superotemporal vs superonasal). Available at: https://www.canadianjournalofophthalmology.ca/article/S0008-4182(07)80124-4/fulltext (Accessed July 2025)

