If you’ve had a stroke in the past and now find yourself dealing with cataracts, you’re not alone—and you’re right to be asking questions. Cataracts can seriously affect your quality of life, but if you’ve already been through the trauma of a stroke, the idea of undergoing eye surgery may seem overwhelming. This article is here to guide you through exactly what to expect and what special considerations might apply to your case.
We’re going to explore how previous strokes—especially those that have affected your visual field or cognitive function—can change how your cataract surgery is planned, performed, and followed up. This includes issues like hemianopia (a type of partial blindness), problems with understanding or giving consent, and even how your body is positioned during surgery.
Understanding the Link Between Stroke and Vision Loss
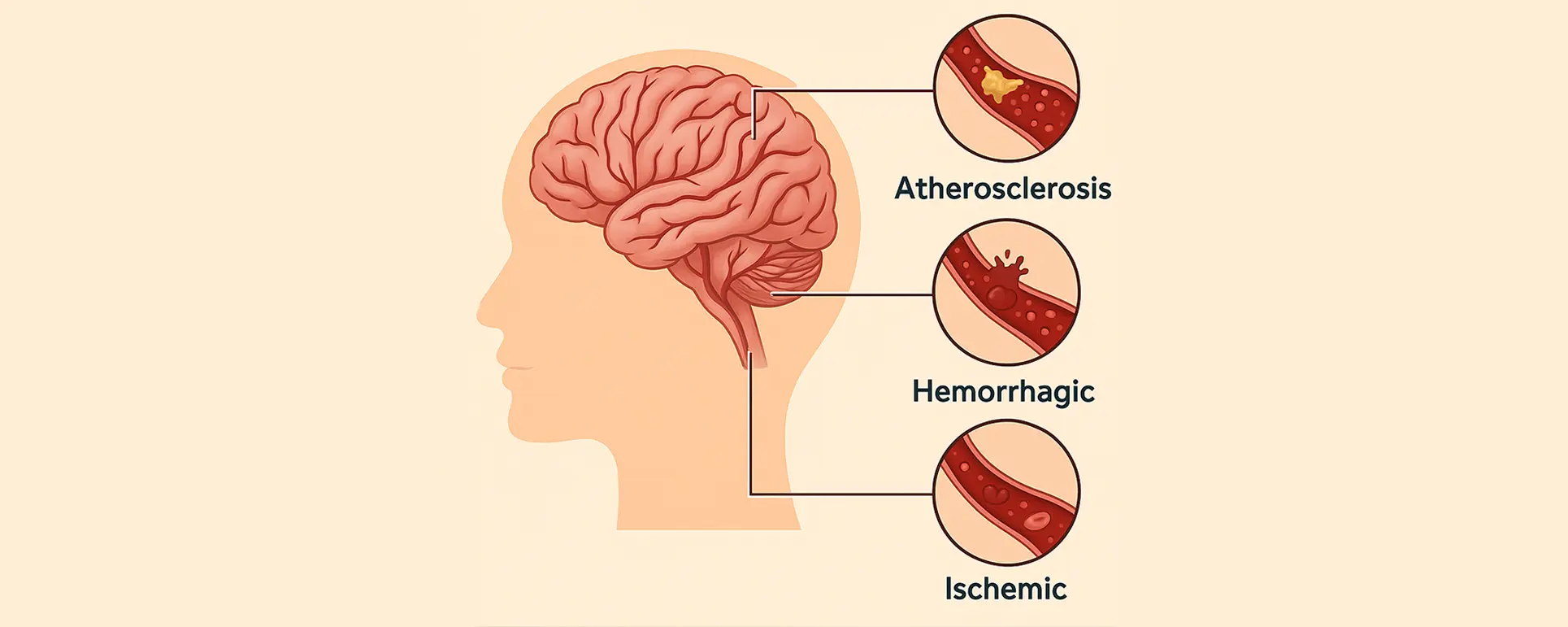
Strokes can affect various parts of the brain, and when they hit the areas responsible for processing visual information, the result is often some form of visual impairment. This could range from blurred vision to more profound issues like hemianopia—where you lose half of your visual field in both eyes.
This kind of visual field loss can be particularly challenging when paired with cataracts. Why? Because cataracts already reduce contrast sensitivity and blur your vision. If you’re already not seeing clearly due to stroke-related damage, cataracts can push your vision below the threshold of functional sight. For some, that can mean the difference between living independently and needing full-time care.
Moreover, because visual field loss is often not noticed by patients themselves—especially if it’s on one side—you might not even realise how badly it’s affecting your daily activities until a proper visual field test is done.
Hemianopia and Cataract Surgery: Unique Visual Challenges
Let’s dive deeper into hemianopia. This is when one half of your visual field—left or right—is lost, typically as a result of a stroke affecting the occipital lobe or optic tract. The real problem during cataract surgery is not so much the operation itself, but what comes before and after it.
- Preoperative Testing
Patients with hemianopia can struggle with basic diagnostic tests such as visual acuity measurements or reading off a Snellen chart. They may also find visual field testing difficult to complete reliably. That can make preoperative planning more complicated. For instance, if a patient cannot fixate properly during optical biometry or OCT scanning, the quality of the data captured may be poor, which in turn can affect IOL power calculation. - Intraoperative Concerns
Surgeons need to understand how the patient’s hemianopia may influence their cooperation during surgery. Even under local anaesthesia, a lack of awareness of one side of the visual field can cause confusion or anxiety during the operation. Also, if the stroke has affected eye movement or caused gaze palsy, keeping the eye steady under the microscope can be trickier. - Postoperative Navigation
After surgery, the gains from improved central vision may still be limited by persistent field loss. Patients must be assessed carefully to avoid disappointment. They also need help understanding how to use their remaining vision effectively, perhaps with the help of low vision aids or occupational therapy.
Communication Barriers: Stroke-Induced Aphasia
Stroke survivors often suffer from aphasia—an impairment in the ability to understand or use language. This presents a major challenge when discussing surgical risks, benefits, and alternatives.
Informed Consent
For any surgical procedure, informed consent is a legal and ethical requirement. But how can you give valid consent if you struggle to understand medical language or can’t communicate your questions or concerns?
Here’s where things get delicate. In patients with aphasia, extra time needs to be taken to explain things using visual aids, simplified language, and repetition. In some cases, a speech and language therapist may be brought in to support the process. When comprehension is severely impaired, surgeons may need to involve legal representatives or family members with power of attorney.
Tailoring the Consultation
A thoughtful surgeon will take a patient-centred approach, slowing down, pausing often, and using more gestures and visual cues. Written information in larger font with diagrams can be helpful, and follow-up consultations may be spaced out to help with memory retention.
This is not just about ticking boxes for legality—it’s about treating the patient with dignity and ensuring they truly understand what’s being proposed.
Positioning Limitations During Surgery

Another thing stroke can leave behind is physical weakness, often on one side of the body (hemiparesis), or more generalised mobility challenges. This becomes highly relevant during cataract surgery, where you need to lie flat and still for up to 30 minutes.
Positioning Challenges
Patients with limited neck mobility, tremors, or weakness may find this position uncomfortable or even unsafe. In such cases, surgeons and anaesthetists need to plan ahead. This could mean elevating the headrest, adding lateral support to prevent rolling, or providing extra pillows and cushions.
Sometimes, sedation must be fine-tuned to relax the patient just enough to remain still without causing respiratory depression—especially important in stroke patients with a history of breathing or swallowing difficulties.
Use of Adjustable Surgical Chairs
Modern ophthalmology clinics often have motorised, adjustable chairs that allow for a customised position. This flexibility can make all the difference for patients with physical impairments, ensuring their comfort and safety throughout the procedure.
Cognitive Considerations After Stroke
Cognitive impairment is common following a stroke, even in patients who seem to recover well physically. Memory issues, poor executive functioning, and difficulty processing new information are all part of the picture.
Planning Around Memory and Attention
These cognitive deficits can affect the ability to follow pre-op and post-op instructions—like when to use eye drops or how to avoid rubbing the eye. Forgetting to take medication or failing to attend follow-up appointments can put surgical outcomes at risk.
Family members or carers often need to be involved at every stage of the process. Providing written instructions in clear language and following up with reminder calls or texts can help reduce risk.
Adjusting Expectations
It’s also important to have honest conversations about visual expectations. A patient who has had a stroke may never regain full visual function, even with perfect cataract surgery. Setting realistic goals is crucial for patient satisfaction.
Anaesthetic Planning and Stroke Risk

Patients with a history of stroke are at higher risk of cardiovascular events. This means their anaesthetic must be planned carefully to avoid triggering another incident.
- Local vs General Anaesthesia
Most cataract operations are performed under local anaesthesia, which is generally safer for stroke patients. However, if communication is severely impaired or the patient is likely to move, sedation or even general anaesthesia may be considered. The anaesthetist must balance the need for patient cooperation with the risk of hypotension or hypoxia—both of which can worsen brain injury. - Cardiovascular Monitoring
Preoperative ECGs, blood pressure management, and ensuring good oxygenation are standard for stroke patients. Some may need pre-op clearance from a neurologist or cardiologist depending on the severity and recency of their stroke.
Postoperative Support and Recovery Challenges
Even with a technically perfect surgery, stroke patients often require more postoperative support than others.
Delayed Recovery and Visual Adaptation
Brain plasticity after a stroke varies widely. Some patients adapt quickly to changes in visual input after surgery. Others, especially those with visual neglect or parietal lobe damage, may find the new clarity from cataract surgery confusing or overwhelming.
Visual rehabilitation may be necessary in the form of orthoptics, prism therapy, or adaptive strategies from low vision specialists.
Transportation and Follow-Up
Getting to and from the clinic for follow-ups can be a challenge if you can’t drive or don’t have easy access to assistance. Hospitals and eye units need to work more closely with community support services to ensure no one falls through the cracks during recovery.
Ethical Considerations and Capacity Assessments
When cognitive or communicative function is significantly impaired, assessing a patient’s capacity to consent becomes ethically complex.
Who Makes the Decision?
If the patient cannot understand or retain information about the surgery, then under UK law, a formal capacity assessment must be carried out. If they are deemed to lack capacity, decisions must be made in their best interest—often by a carer with legal authority or by a multidisciplinary team.
This is particularly sensitive in eye care, where the procedure is often elective but can profoundly improve independence. Ethical discussions around quality of life, autonomy, and dignity come into play.
Holistic Care: Multidisciplinary Planning
Stroke survivors are rarely dealing with just one issue. Cataract surgery for these patients is most successful when approached as a team effort.
- Ophthalmologist – leads the surgical planning and visual assessment.
- Neurologist – advises on stroke-related risks.
- Anaesthetist – ensures safety during the procedure.
- Speech and language therapist – helps with communication and consent.
- Occupational therapist – supports visual adaptation and independence.
- Carers or family – reinforce aftercare and support decision-making.
When all these elements work together, patients with a history of stroke can have very successful outcomes with cataract surgery.
FAQs: Cataract Surgery in Patients with Stroke History
- Can I still have cataract surgery if I’ve had a stroke?
Yes, most stroke survivors can safely undergo cataract surgery, but it does require more careful planning. Your surgical team will consider any vision changes, mobility issues, communication difficulties, and cognitive challenges you may have following the stroke. With the right support and preparation, many patients with stroke history go on to have very successful outcomes. - What is hemianopia, and how does it affect cataract surgery?
Hemianopia is when you lose half of your visual field—usually on the left or right side—often as a result of a stroke. While cataract surgery can help clear up central vision, it won’t restore the part of your vision that was lost due to stroke. However, surgery can still greatly improve your overall visual function and quality of life, especially if the cataract is significantly clouding your remaining vision. - Will my stroke-related memory or speech problems affect my ability to consent?
They might, but your care team will assess this thoroughly. If you have difficulty understanding information or expressing yourself clearly, your team may use pictures, simple explanations, or involve speech and language therapists to support you. If you’re unable to give informed consent due to cognitive issues, a legal representative or someone with lasting power of attorney may be needed to help make decisions in your best interest. - What if I can’t lie flat for the operation due to stroke-related weakness?
Many patients who’ve had a stroke have mobility challenges or discomfort when lying down flat. Your surgical team can adjust the operating chair or use extra supports like pillows to make you comfortable. If you still struggle, sedation or anaesthetic adjustments may be made so that you can stay relaxed and still during the procedure. - Is there a higher risk of complications if I’ve had a stroke before?
Having a stroke in your medical history does increase some risks, particularly cardiovascular ones like blood pressure instability or poor blood flow during surgery. That’s why stroke survivors usually have more pre-op checks, like heart assessments and anaesthetic reviews. The aim is to ensure the procedure is as safe and low-risk as possible based on your individual health profile. - Can stroke-related visual problems be corrected during cataract surgery?
Cataract surgery only addresses the lens of your eye—it doesn’t treat damage in the brain caused by a stroke. So, if your visual issues are due to a stroke (like field loss or double vision), they may remain. But improving the clarity and contrast of your remaining vision by removing a cataract can still make a big difference in how well you function day to day. - What support will I need after cataract surgery if I’ve had a stroke?
You’ll likely need more help than the average patient. This could include reminders to take eye drops, assistance attending follow-up visits, and help adjusting to your improved vision. If you have memory problems or struggle with instructions, having a family member or carer closely involved can really improve your chances of a smooth recovery. - Should I delay surgery if my stroke was recent?
It depends on your recovery status. If your stroke was very recent—within the last 3 months—your surgical team may advise waiting until you’re more stable. However, if your vision is badly impaired and you’re otherwise medically cleared, earlier surgery may still be appropriate. Each case is assessed individually to balance safety with quality of life. - Will cataract surgery affect my rehabilitation from stroke?
In many cases, clearer vision can actually help with stroke rehabilitation, especially for tasks like walking, reading, or recognising faces. However, it’s essential to coordinate with your stroke rehabilitation team, particularly if you’re receiving occupational therapy or using visual cues for mobility. Improving your eyesight can support your recovery, but the timing should be carefully planned. - What should I tell my eye surgeon about my stroke?
Be as open as possible about your stroke history—when it happened, which side of the body was affected, any speech or memory issues, and whether you have any vision problems like field loss or double vision. Also let them know about medications you’re taking, especially blood thinners or heart-related drugs. The more your surgeon knows, the safer and more tailored your care will be.
Final Thoughts
Having had a stroke doesn’t mean cataract surgery is off the table—but it does mean you and your surgical team need to go the extra mile to prepare. From understanding visual field deficits like hemianopia, to accommodating communication barriers, cognitive changes, and physical limitations, there’s a lot to think about.
But when done thoughtfully, cataract surgery can make a tremendous difference to your independence, safety, and quality of life—even if your vision will never be “perfect.” It’s all about tailoring the approach to your needs, being honest about outcomes, and surrounding you with the right support at every step.
References
1. NHS. (2022). Cataract surgery. Retrieved from
https://www.nhs.uk/conditions/cataract-surgery/
2. Rowe, F.J., Wright, D., Brand, D. et al. (2013). A prospective profile of visual field loss following stroke: prevalence, type, rehabilitation, and outcome. BioMed Research International, 2013, Article ID 719096. Retrieved from
https://www.hindawi.com/journals/bmri/2013/719096/
3. Royal College of Ophthalmologists. (2020). Standards of Consent for Ophthalmology Procedures (including cataract). Retrieved from
https://www.rcophth.ac.uk/wp-content/uploads/2020/05/Standards-Of-Consent-For-Ophthalmology-Procedures-COVID-19.pdf
4. Stroke Association. (n.d.). Vision problems after stroke. Retrieved from
https://www.stroke.org.uk/stroke/effects/physical/vision-problems-after-stroke
5. Stroke Association. (n.d.). Support with vision problems after stroke. Retrieved from
https://www.stroke.org.uk/stroke/effects/physical/vision-problems-after-stroke/support-with-vision-problems