If you or someone close to you has been told they have cataracts, you’re certainly not alone. Cataracts are incredibly common, especially as we age. But thanks to medical advancements, the solution is now faster, safer, and more effective than ever before. One word you’ll probably hear a lot during this journey is phacoemulsification. It might sound a bit intimidating, but don’t worry—I’m going to walk you through everything in plain, simple language.
So let’s dive into what phacoemulsification really is, why it’s become the gold standard for cataract surgery, and what you can expect every step of the way.
What Exactly Is Phacoemulsification?
Phacoemulsification (or just phaco for short) is a modern surgical technique used to remove cataracts from the eye. A cataract is simply a clouding of the natural lens, which affects how clearly you see. In phacoemulsification, your eye surgeon uses a tiny ultrasonic device to break up the cloudy lens into smaller fragments. These are then suctioned out, and a new artificial lens (called an intraocular lens, or IOL) is inserted in its place.
The real magic here is how minimally invasive it all is. There are no stitches in most cases, and the incision is so small that it often heals on its own.
A Brief Look at the History of Cataract Surgery
Before phacoemulsification came along, cataract surgery was a lot more involved. Surgeons had to make larger incisions and physically remove the entire cloudy lens in one piece. Recovery times were longer, complications more common, and patients often had to wear thick glasses afterwards to correct their vision.
In the late 1960s, a surgeon named Dr Charles Kelman introduced phacoemulsification to the world. His idea was inspired by a dentist’s ultrasonic drill, and it revolutionised cataract surgery completely. From that point forward, smaller incisions, quicker healing, and better outcomes became the norm.
Why Phacoemulsification Has Become the Standard
There’s a good reason this technique is used in the vast majority of cataract surgeries today. Let’s look at the advantages in a bit more detail.
It’s Minimally Invasive
Tiny incisions mean minimal trauma to the eye. That leads to less inflammation, faster healing, and fewer complications.
Recovery Time is Much Quicker
In most cases, patients are back to their normal routine within a few days. You might still need to take it easy for a week or so, but gone are the days of extended recovery.
Precision is Key
Modern phacoemulsification systems are incredibly precise. This allows surgeons to target just the cloudy lens and leave the surrounding tissue untouched.
Excellent Visual Outcomes
With the right intraocular lens choice, many patients end up seeing even better than before they developed cataracts—sometimes even without glasses.
The Step-by-Step Phacoemulsification Procedure
Let’s break down what actually happens during a phacoemulsification procedure. It’s not as scary as it sounds—promise. Understanding each step can take away a lot of the mystery and anxiety. Once you know what’s involved, you’ll see just how far modern medicine has come in making eye surgery quick, comfortable and highly effective.
This isn’t some old-fashioned approach where you’re knocked out for hours and left recovering for weeks. In fact, phacoemulsification is a minimally invasive, outpatient procedure that usually takes less than half an hour. You’re awake the whole time, but completely comfortable—and most people are surprised by how smooth and straightforward it all is.
Here’s what you can expect, step by step, when undergoing phacoemulsification. From the initial numbing of your eye to the moment you walk out of the clinic, it’s all designed to be as gentle and efficient as possible.
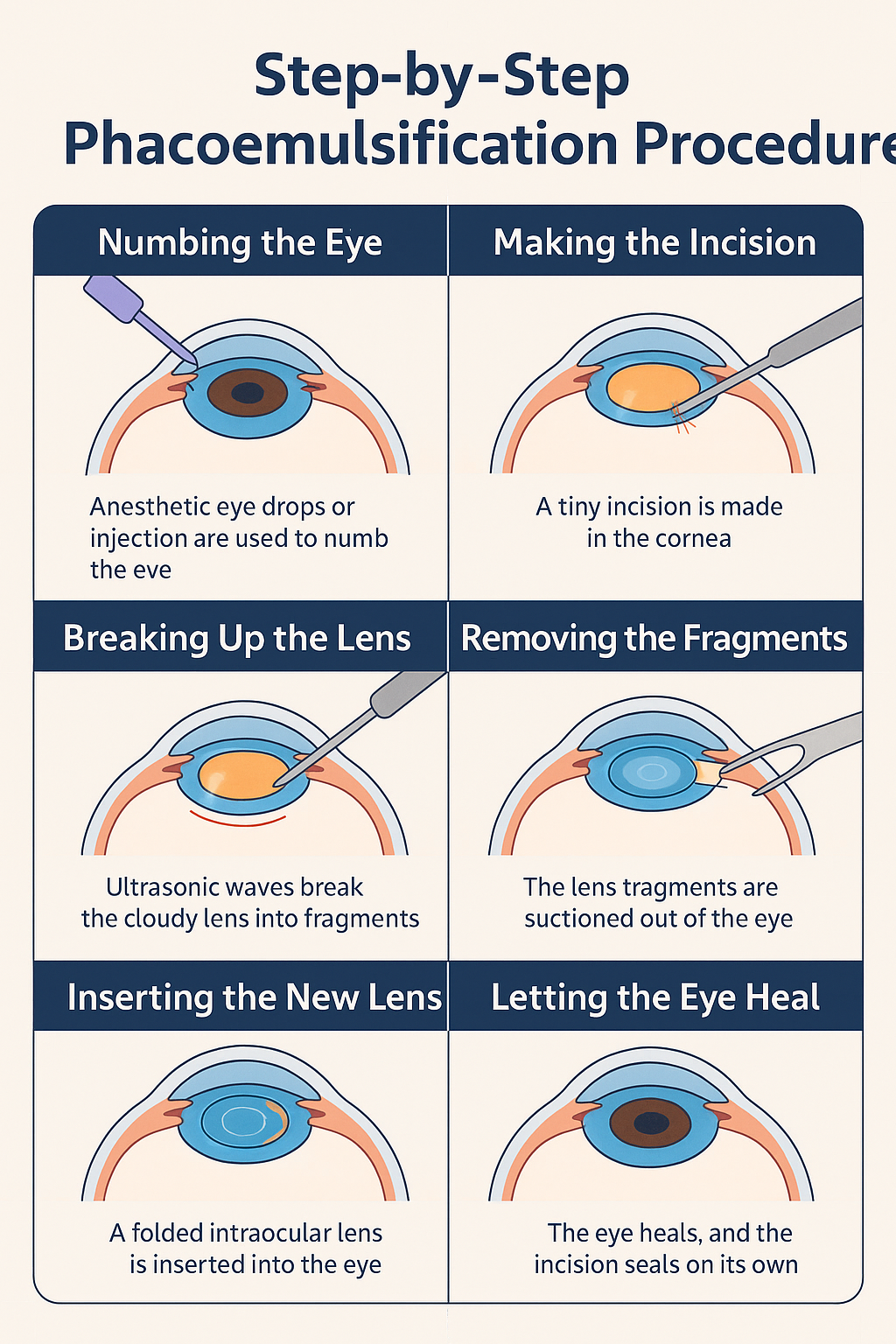
Step 1: Numbing the Eye
The first step is making sure you don’t feel any discomfort during the surgery. This is done using local anaesthesia, either in the form of numbing eye drops or, occasionally, a small injection near the eye. It might sound unsettling, but the drops work very quickly and you won’t feel anything sharp or painful—just a slight sting that fades in seconds.
Once the anaesthetic kicks in, the entire surface of the eye becomes completely desensitised. You may still sense a bit of pressure or vague movement during the procedure, but you won’t experience pain. Some clinics also offer a mild sedative if you’re particularly anxious, helping you to feel calm and relaxed throughout.
Importantly, since you’re awake during the operation, your surgeon can guide you gently and keep you informed as they go. That means you’re never in the dark—figuratively speaking, of course. You might see bright lights or blurry shapes, but it’s all very manageable, and the team will be there to support you every step of the way.
Step 2: Making the Incision
Once your eye is fully numb, the surgeon makes a tiny incision on the surface of the cornea. This incision is incredibly small—typically just 2 to 3 millimetres—so there’s very little disruption to the eye’s structure. Despite how delicate it sounds, this step is remarkably precise, thanks to modern surgical tools and imaging technology.
The small size of the incision means that it’s often self-sealing. In other words, it closes up naturally without the need for stitches. This greatly reduces the risk of infection and promotes faster healing, which is a big reason why recovery times for phacoemulsification are so short compared to older surgical methods.
The placement of the incision is also carefully considered. Surgeons aim to position it in a way that avoids sensitive parts of the eye and creates minimal visual distortion after surgery. This thoughtful planning plays a huge role in the smooth recovery and excellent vision most patients experience post-op.
Step 3: Breaking Up the Lens
With the incision made, the surgeon now needs to address the cataract itself. This is where phacoemulsification earns its name. A tiny probe is inserted into the eye through the incision, and it uses high-frequency ultrasonic energy to break the cloudy lens into microscopic pieces. It’s a clever use of sound waves that gently disintegrates the lens without damaging nearby tissues.
The ultrasound energy is carefully controlled and modulated throughout the process. Surgeons can adjust the intensity in real time, depending on the density of the cataract. Softer cataracts may require less energy, while harder or more advanced cataracts might take a little more time and precision to break down fully.
This step is crucial, as it allows the surgeon to remove the cataract through a tiny incision, instead of needing to extract it whole. The technology involved is impressively sophisticated, allowing for clean fragmentation and minimal trauma to the surrounding eye structures. The result? A safer procedure and quicker recovery for you.
Step 4: Removing the Fragments
After the cataract has been broken up, the next job is to remove all those tiny lens fragments. Thankfully, the same instrument that delivered the ultrasound energy also acts as a vacuum. It gently suctions out the debris, making sure nothing is left behind to cloud your vision later.
This stage requires a delicate balance. Too much suction could disturb other parts of the eye, while too little could leave fragments behind. Modern phaco machines are designed to maintain this balance with exceptional accuracy, constantly monitoring intraocular pressure and flow rate during the removal process.
The goal here is to leave the capsular bag (the natural structure that held your original lens) intact. This bag will house your new artificial lens, and preserving it helps ensure your vision remains stable and centred once the new lens is in place. It’s a process that’s both intricate and elegant in its design.
Step 5: Inserting the New Lens
Now that the old, cloudy lens has been removed, it’s time to insert the new intraocular lens (IOL). These artificial lenses are usually made of soft, foldable materials. They’re cleverly designed to be rolled up and inserted through the same small incision, before unfolding perfectly inside the eye.
Your surgeon will have already selected the right lens type and power for your needs, based on pre-surgery measurements. Once inside the eye, the IOL is positioned in the capsular bag, right where your natural lens used to sit. It’s a snug fit, and the flexible ‘arms’ of the lens (called haptics) help keep it securely in place.

What’s impressive is how seamlessly this step is performed. The lens unfolds naturally, without any force, and settles into position with minimal handling. There’s no need for sutures or glue—everything relies on the precision of placement and the natural anatomy of your eye to hold it steady.
Step 6: Letting the Eye Heal
With the new lens in place, the surgeon gives the eye a final rinse with a sterile solution, checking to ensure everything is clear and stable. Because the incision is so tiny, it doesn’t usually need to be stitched closed. The eye’s natural pressure helps seal it shut, which speeds up healing and reduces the risk of complications.
After the procedure, you’ll rest for a short while before heading home. Your eye may feel slightly gritty or sensitive for a few hours, but most people find it very manageable. You’ll be given post-op instructions, including how to use your eye drops and what signs to watch for during the healing process.
Healing is usually quick and uneventful. Most patients notice better vision within a few days, though it can take a week or two to reach the final result. You’ll have follow-up appointments to make sure your eye is healing properly, and before you know it, you’ll be seeing the world more clearly than you have in years.
The Role of Intraocular Lenses (IOLs)
The new lens that replaces your old, cloudy one is critical to the success of the surgery. There are several types of IOLs available today, and your surgeon will help you choose the one that suits your lifestyle and visual needs.
Monofocal Lenses
These are the standard IOLs provided by the NHS. They offer clear vision at one distance—usually for distance viewing—so you might still need reading glasses.
Multifocal Lenses
These provide vision at multiple distances, reducing your dependence on glasses. They do come with a higher price tag, and may cause some halo effects around lights at night.
Toric Lenses
If you have astigmatism, toric lenses are designed to correct it while also treating your cataract.
Choosing the right IOL is a very personal decision and can significantly affect how satisfied you are with your post-surgery vision. Always have a proper discussion with your eye surgeon about this.
What to Expect Before the Surgery
You’ll have a thorough consultation, which includes measurements of your eye and discussions about your medical history, medications, and vision goals. The measurements help decide the power of the new lens you’ll receive.
A week or two before surgery, you’ll be given pre-operative instructions. This might include stopping certain medications or using eye drops to prevent infection.
What Happens on the Day?
You’ll come into the clinic or hospital, have your eye numbed, and get prepped for the procedure. Most people are in and out within a few hours. You’ll need someone to drive you home, though.
You won’t feel pain during the surgery, but you might see bright lights or some vague movement. It’s more weird than uncomfortable, really.
Post-Operative Recovery: The Do’s and Don’ts
After the procedure, you’ll be given eye drops to use for a few weeks. These usually include antibiotics and anti-inflammatories. You’ll also be given a protective eye shield to wear at night for a few days.
The Do’s
- Do use your eye drops exactly as instructed.
- Do rest your eyes and take it easy.
- Do attend your follow-up appointments to make sure everything’s healing properly.

The Don’ts
- Don’t rub your eye.
- Don’t go swimming or use hot tubs for at least a couple of weeks.
- Don’t wear eye makeup or do strenuous exercise right away.
Your vision might be blurry for a few days, but most people start seeing an improvement very quickly. Colours seem brighter, contrast is sharper, and everything just looks clearer.
Are There Any Risks?
As with any surgery, phacoemulsification does carry some risks, but they’re relatively rare. Here are a few possibilities:
Infection (Endophthalmitis)
It’s extremely uncommon, especially with modern sterile techniques, but it can be serious. That’s why post-op eye drops and hygiene are so important.
Posterior Capsule Opacification (PCO)
This is the most common delayed complication and happens when the membrane behind the new lens becomes cloudy. If it does happen, it’s easily fixed with a quick, painless laser procedure called YAG capsulotomy.
Retinal Detachment or Macular Oedema
Both are rare but can affect vision. You’ll be monitored for any signs in the follow-up period, and early treatment usually leads to good outcomes.
Who is (and Isn’t) a Good Candidate?
Phacoemulsification is suitable for the vast majority of patients with age-related cataracts. However, there are a few situations where your surgeon might opt for a different technique.
Good Candidates
- Age-related cataracts
- Clear corneas and healthy retina
- Desire for a quick recovery

Caution Needed
- Very dense cataracts
- Pre-existing corneal disease
- Small pupils that don’t dilate well
Your surgeon will do a full assessment and decide whether phaco is right for you, or whether a slightly different approach is needed.
Innovations in Phacoemulsification
Modern phaco machines are much more advanced than the original 1960s versions. Today, they come with computer-guided controls, energy modulation, and even femtosecond laser integration for added precision.
In some cases, laser-assisted cataract surgery is used alongside phacoemulsification to create even more precise incisions and reduce the amount of ultrasound energy needed.
Some machines even adjust in real time to changes in your eye pressure, helping to maintain a very stable environment during surgery. It’s all pretty impressive.
Final Thoughts: Should You Be Worried?
Not at all. If you’re facing cataract surgery, phacoemulsification is likely the method your surgeon will use—and with good reason. It’s safe, effective, and has a proven track record of excellent visual outcomes.
It’s perfectly normal to feel nervous before any procedure involving your eyes, but millions of people go through this surgery every year with overwhelmingly positive results. Ask your questions, discuss your lens options, and make sure you feel comfortable with your surgical team.
If you’re considering private cataract surgery in London, you’re welcome to get in touch with us at the London Cataract Centre to arrange a consultation with one of our expert cataract surgeons.
By the time you’re out the other side, chances are you’ll wonder why you ever worried in the first place.

