When you think about cataract surgery, you probably imagine it as a straightforward swap: your cloudy natural lens is removed, and a clear artificial one takes its place. That picture isn’t wrong, but it also doesn’t tell the whole story. Intraocular lenses, or IOLs, have been evolving for decades, and we’re now standing on the edge of another major leap forward. This leap comes from nanotechnology and smart materials—fields of science that are quietly reshaping how we think about vision correction after cataracts.
If you’ve heard the buzzwords “nano” and “smart” before, you might associate them with electronics, textiles, or even car paint. But the truth is, these technologies are now being directed at something much closer to us—our eyes. Researchers are exploring how nanostructures and responsive materials could make the next generation of IOLs more resilient, more adaptable, and more in tune with the way our eyes actually work.
So in this article, let’s explore what nanotechnology really means for IOLs, what smart materials could do in the context of cataract surgery, the current research being done, and the very real challenges that stand in the way. By the end, you’ll have a picture of how tomorrow’s lenses could differ radically from today’s—and why that matters to anyone facing cataract surgery in the years to come.
Why Today’s Intraocular Lenses Still Have Limits
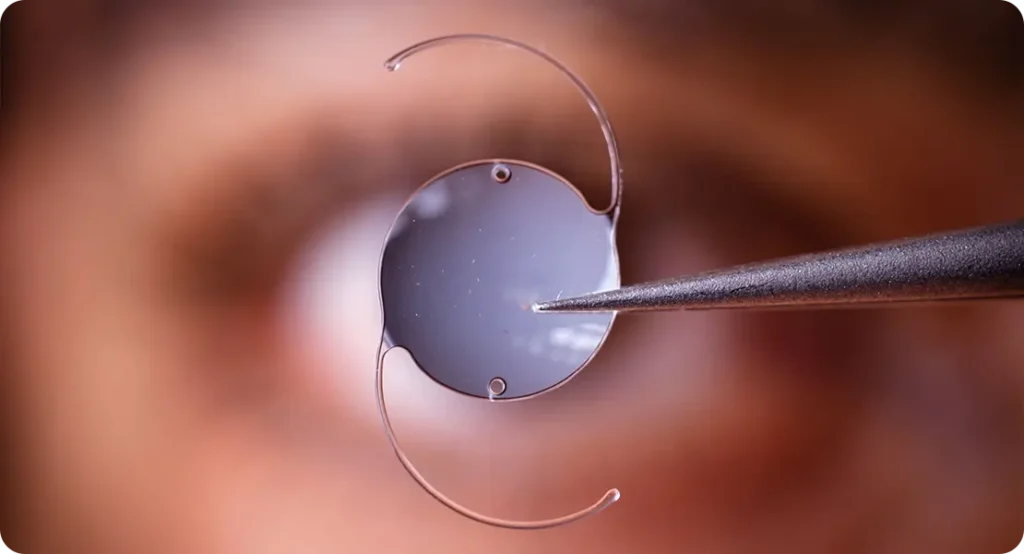
Modern IOLs are a triumph of medical engineering. They’re tiny, durable, and they sit quietly in the eye for decades, restoring vision that cataracts had stolen. But they aren’t perfect.
For one thing, they’re essentially static. A monofocal IOL restores vision at a single distance. A multifocal or trifocal lens allows vision across several ranges, but they still rely on fixed optics. They don’t actively adjust themselves in response to your environment.
There are also issues with long-term clarity. Some lenses develop tiny imperfections known as glistenings, which scatter light and reduce contrast. Others may be prone to deposits on their surface, or they may provoke the body’s natural healing response, which can lead to posterior capsule opacification (often referred to as a “secondary cataract”).
And then there’s infection. Although post-surgical infection is very rare, when it happens it can be devastating. Any improvement in the lens’ ability to resist bacterial colonisation is a win.
This is why scientists are asking: what if lenses could do more? What if they could adapt, resist, protect, and even respond to the environment inside your eye?
Enter Nanotechnology
Nanotechnology is about working with materials at an incredibly small scale—so small that it’s measured in nanometres (one billionth of a metre). At this level, the behaviour of a material can change. Surfaces may become more water-repellent, more transparent, or more biocompatible. By manipulating a lens at the nanoscale, researchers can give it properties that a normal polymer simply doesn’t have.
Applied to intraocular lenses, nanotechnology opens up several exciting possibilities.
Self-Cleaning Surfaces
One of the challenges with any implanted medical device is keeping it free of deposits and unwanted cell adhesion. Nanostructures can be engineered so that proteins, lipids, and cells simply don’t stick. A self-cleaning IOL wouldn’t gather deposits that blur vision, reducing the risk of secondary cataracts.
Antimicrobial Protection
Silver nanoparticles and other antimicrobial agents at the nanoscale are already used in wound dressings and coatings. Applied to an IOL, they could create a hostile environment for bacteria, drastically lowering the risk of post-operative infection.
Reduced Glistenings
By controlling the polymer structure at a molecular level, it’s possible to prevent the microvacuoles that cause glistenings. Patients could enjoy clearer vision for decades without the tiny imperfections that sometimes plague current lenses.
Precision Light Filtering
Blue-light filtering IOLs already exist, but nanotechnology could refine this dramatically. Imagine a lens that selectively blocks harmful UV or high-energy blue light while allowing the full spectrum of useful light through, preserving both colour perception and retinal protection.
Better Biocompatibility
The eye can sometimes treat an IOL as a foreign object. Nanostructures that mimic natural tissue can reduce inflammation and improve integration, meaning smoother recovery and longer-lasting comfort.
The Role of Smart Materials

If nanotechnology is about enhancing material properties, smart materials go one step further. These are materials that change in response to a stimulus—light, heat, electrical current, or even chemical changes in the eye.
This is where things start to get really interesting for IOLs.
Light-Responsive Polymers
Think about glasses that darken in sunlight and lighten indoors. Now imagine that built into your IOL. Light-responsive polymers could allow a lens to adapt its transmission in real time, reducing glare outdoors while staying clear indoors.
Shape-Memory Materials
These materials can change shape when stimulated. For IOLs, that could mean a lens that fine-tunes its curvature based on temperature or mechanical signals, potentially restoring some degree of natural accommodation.
Electro-Active Lenses
This is still futuristic, but it’s not just theory. Electro-active polymers can alter their optical properties when a tiny electrical current is applied. If technology advances far enough, an electro-active IOL could actively change its focus point depending on where you’re looking.
Biochemical Sensors
Smart coatings might even respond to the chemistry of the eye. Inflammation? The lens surface could release a soothing agent. Fluctuations in tear film? The lens could subtly alter its hydrophilic properties.
The Potential Benefits for Patients
It’s worth asking: why does all this matter? After all, cataract surgery already delivers life-changing results. The answer is that these innovations could address the few remaining pain points in cataract outcomes.
- Lower complication rates: Antimicrobial and self-cleaning surfaces could reduce infections and secondary cataracts.
- Better long-term clarity: Eliminating glistenings and deposits means consistently sharp vision for life.
- Dynamic visual performance: Smart lenses could provide personalised adaptation to different lighting conditions and visual tasks.
- Improved comfort and recovery: With better biocompatibility, eyes may heal faster and experience fewer inflammatory reactions.
- Closer to natural vision: By restoring some of the eye’s lost ability to adapt, smart IOLs could mimic the behaviour of the natural crystalline lens more closely than ever before.
Where Are We Right Now?
It’s important to be realistic. Most of these technologies are still in the research or early trial phase. Nanocoatings for antimicrobial protection are perhaps the furthest along, with several studies showing promise. Light-responsive materials and electro-active lenses are still experimental prototypes.
The main challenge is durability. An IOL needs to last decades without degrading. A lens that works beautifully for five years but then loses its functionality isn’t good enough. Researchers must prove not only that these lenses work, but that they remain safe and effective for the long haul.
And then there are regulatory hurdles. Medical devices like IOLs undergo rigorous approval processes. It could take many years before nanotechnology- or smart-material-based IOLs are available outside of research settings.
The Challenges Ahead
Bringing these innovations to patients isn’t straightforward. Some of the biggest challenges include:
- Longevity of function – Can a smart material still perform after 20 years in the eye?
- Power requirements – For electro-active lenses, how do you provide safe, long-term power?
- Manufacturing scale – Can nanostructures be mass-produced consistently and affordably?
- Safety – How do we guarantee nanoparticles or new polymers won’t cause harm decades later?
- Regulatory approval – The process is slow, expensive, and essential to ensure safety.
Looking Ahead: The Next 10–20 Years
So what might the future look like? It’s possible that in the next couple of decades, cataract patients will have a menu of options:
- Conventional lenses – Tried-and-true acrylic or silicone IOLs.
- Nanotech-enhanced lenses – With self-cleaning and antimicrobial properties.
- Smart adaptive lenses – Light-responsive, shape-shifting, or electro-active lenses that restore aspects of natural accommodation.
Just as multifocal IOLs went from experimental to mainstream, we may see nanotech and smart IOLs follow a similar trajectory. The difference is that these innovations have the potential not just to improve vision, but to redefine what an artificial lens can be.
FAQ: Nanotechnology and Smart Materials in Intraocular Lenses
1. What is nanotechnology in IOLs?
Nanotechnology in intraocular lenses refers to the use of materials and surface structures engineered at the scale of nanometres, which is a billionth of a metre. At this level, the physical and chemical behaviour of materials can be radically different compared to their bulk form. For IOLs, nanotechnology allows surfaces to be designed that resist deposits, reduce bacterial growth, filter light more precisely, and improve how the lens interacts with living tissue. In practice, this could mean a lens that stays clearer for longer, heals more smoothly within the eye, and provides better vision over a patient’s lifetime.
2. How could self-cleaning IOLs help patients?
Self-cleaning IOLs use nanostructured surfaces that are specifically designed to repel proteins, lipids, and even cells that would normally attach themselves to the lens. Over time, these deposits are one of the causes of cloudiness or “secondary cataract,” also known as posterior capsule opacification. By preventing such build-up from occurring in the first place, self-cleaning IOLs would help patients enjoy consistently clear vision for decades without the need for additional procedures like YAG laser capsulotomy, which is often used today to clear opacification.
3. Can nanotechnology make lenses safer against infection?
Yes, one of the most exciting applications of nanotechnology in IOLs is antimicrobial protection. Researchers are experimenting with nanoparticles of silver, copper, and other agents that are well known for their ability to kill or suppress bacteria. Applied at the nanoscale, these coatings could create a hostile surface where bacteria cannot thrive, preventing biofilm formation that can lead to infection. While infection after cataract surgery is already rare, these new lenses could lower the risk even further, giving surgeons and patients an extra layer of reassurance.
4. What are glistenings, and how does nanotech address them?
Glistenings are tiny, fluid-filled microvacuoles that can develop inside some types of intraocular lenses. They scatter light within the lens material, reducing contrast sensitivity and in some cases affecting overall visual quality. Although they don’t always cause symptoms, when they do, they can be frustrating for patients. Nanotechnology provides a way to engineer lens polymers with structures that resist the formation of these microvacuoles in the first place. By controlling the material at the molecular level, scientists hope to create lenses that are completely free from glistenings, ensuring consistently sharp vision.
5. Are smart IOLs available now?
At present, no fully functional “smart” intraocular lenses are available commercially. Most of the innovations involving light-responsive materials, electro-active polymers, or shape-memory technologies are still in research and development. There are prototypes that have shown promise in laboratory and early trial settings, but the regulatory pathway for an implant that needs to last inside the eye for decades is understandably long and rigorous. For now, patients can choose between monofocal, multifocal, trifocal, extended depth of focus, and toric lenses, but smart IOLs remain part of the future rather than the present.
6. How do light-responsive IOLs differ from current blue-light lenses?
Current blue-light filtering lenses block a fixed portion of high-energy light at all times, regardless of conditions. Light-responsive IOLs, on the other hand, would be able to change their light transmission dynamically. In bright sunlight, they might darken to reduce glare and protect the retina, and indoors they could return to a clear state for natural colour vision. This adaptability could make vision more comfortable in different environments, something that current static filters cannot achieve.
7. Will smart IOLs need electricity?
Some smart lenses, especially those based on electro-active polymers, do require electrical stimulation to change their shape or focus. This presents a challenge, as powering a device inside the eye safely and reliably for decades is not straightforward. Researchers are exploring options such as harvesting energy from natural eye movements or using tiny wireless systems, but this is still at the prototype stage. Other types of smart IOLs, such as light-responsive or shape-memory polymers, do not require electricity at all, as they change in response to passive environmental triggers like light or temperature.
8. Are nanoparticles safe inside the eye?
This is one of the most carefully studied questions in the field. Nanoparticles behave differently than larger-scale materials, and while many show promise in the lab, long-term safety has to be demonstrated beyond doubt. A lens that sits inside the eye for decades must be proven to remain non-toxic, stable, and biocompatible over the entire lifespan of the patient. Early research suggests that certain nanoparticles, such as silver, can be stabilised in ways that are safe, but until long-term studies confirm this, regulatory approval will not be granted.
9. When might these lenses reach patients?
It’s difficult to put an exact timeline on it, but most experts suggest that nanotechnology-enhanced IOLs with self-cleaning or antimicrobial properties could appear in clinical use within the next 5–10 years. Truly adaptive smart lenses that adjust their optical properties in real time may take longer, perhaps 10–20 years, because the technology is more complex and the safety standards are higher. The regulatory process for medical implants is deliberately cautious, meaning new designs undergo years of rigorous testing before they reach patients.
10. Will these lenses cost more than current IOLs?
Almost certainly, at least in the early stages. New technologies always carry higher development and manufacturing costs, and nanostructures or smart polymers are more complex to produce than standard acrylic lenses. Patients opting for these lenses would likely pay a premium, just as they do today for trifocal or toric lenses compared to basic monofocals. However, if these lenses prove their value by delivering longer-lasting clarity and reduced complications, their cost may be justified. Over time, as production scales and patents expire, the prices are likely to come down, making them more widely accessible.
Final Thoughts
Nanotechnology and smart materials hold the promise of a new era in cataract surgery. The lens of the future won’t just restore vision—it may adapt, protect, and even heal in ways we’ve never seen before.
For patients, that could mean clearer sight for life, fewer complications, and a lens that behaves more like the one nature originally gave you. For surgeons, it means new tools to deliver precision outcomes and push the boundaries of what’s possible in eye care.
The journey isn’t complete yet, but the path is clear. Intraocular lenses are on their way to becoming not just replacements, but truly intelligent companions for vision.
References
- Hu, C.T., Hsu, S.H., Tsai, C.Y., & Chen, W. (2015) ‘Strategic Design of Biocompatible, Glistening-Free, and Foldable Artificial Intraocular Lenses Based on Hydro-Amphiphilic Ternary Copolymers’, Biomacromolecules, 16(6), pp. 1874–1883. Available at: https://pubs.acs.org/doi/10.1021/acs.biomac.5c00588 (Accessed: 22 October 2025).
- Vacalebre, M., La Fauci, L., Musolino, C., & Calogero, A. (2023) ‘Current State of the Art and Next Generation of Materials for a New Generation of Intraocular Lenses’, International Journal of Molecular Sciences, 24(6), 54364. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10054364/ (Accessed: 22 October 2025).
- Wu, K.Y., Lin, C.H., & Chang, J. (2024) ‘Innovative Polymeric Biomaterials for Intraocular Lenses in the Modern Era’, Journal of Functional Biomaterials, 15(12), 391. Available at: https://www.mdpi.com/2079-4983/15/12/391 (Accessed: 22 October 2025).
- Afarid, M., Mahmoodi, S., & Baghban, R. (2022) ‘Recent Achievements in Nano-Based Technologies for Ocular Disease Diagnosis and Treatment: Review and Update’, Journal of Nanobiotechnology, 20, 361. Available at: https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01567-7 (Accessed: 22 October 2025).
- Gonzalez, F., Crespo, J., & Perez, M. (2024) ‘Feasibility of Smart Intraocular Lens: A Pilot Study of Communication Between a Conventional Smartphone and an Intraocular Tag’, Frontiers in Medical Technology, 6, 11246928. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC11246928/ (Accessed: 22 October 2025).

