If you or someone you care about has keratoconus and is now facing cataract surgery, you’re probably wondering—what makes this different? And how do surgeons navigate the challenges to get the best possible vision afterwards? You’re not alone in asking these questions.
Cataract surgery in keratoconic eyes is a tricky intersection between two conditions that each distort vision in their own right. Put them together, and you’ve got a highly individualised scenario where success hinges on meticulous planning, advanced diagnostics, and a solid understanding of how these eyes behave.
In this article, we’ll explore the major challenges in achieving predictable refractive outcomes in keratoconus patients undergoing cataract surgery. We’ll also look at current evidence guiding intraocular lens (IOL) selection, power calculation techniques, and postoperative considerations.
Whether you’re a patient, optometrist, or cataract surgeon, this guide is designed to help you grasp the key clinical decisions that go into making this kind of surgery a success.
Understanding the Basics: What Is Keratoconus?
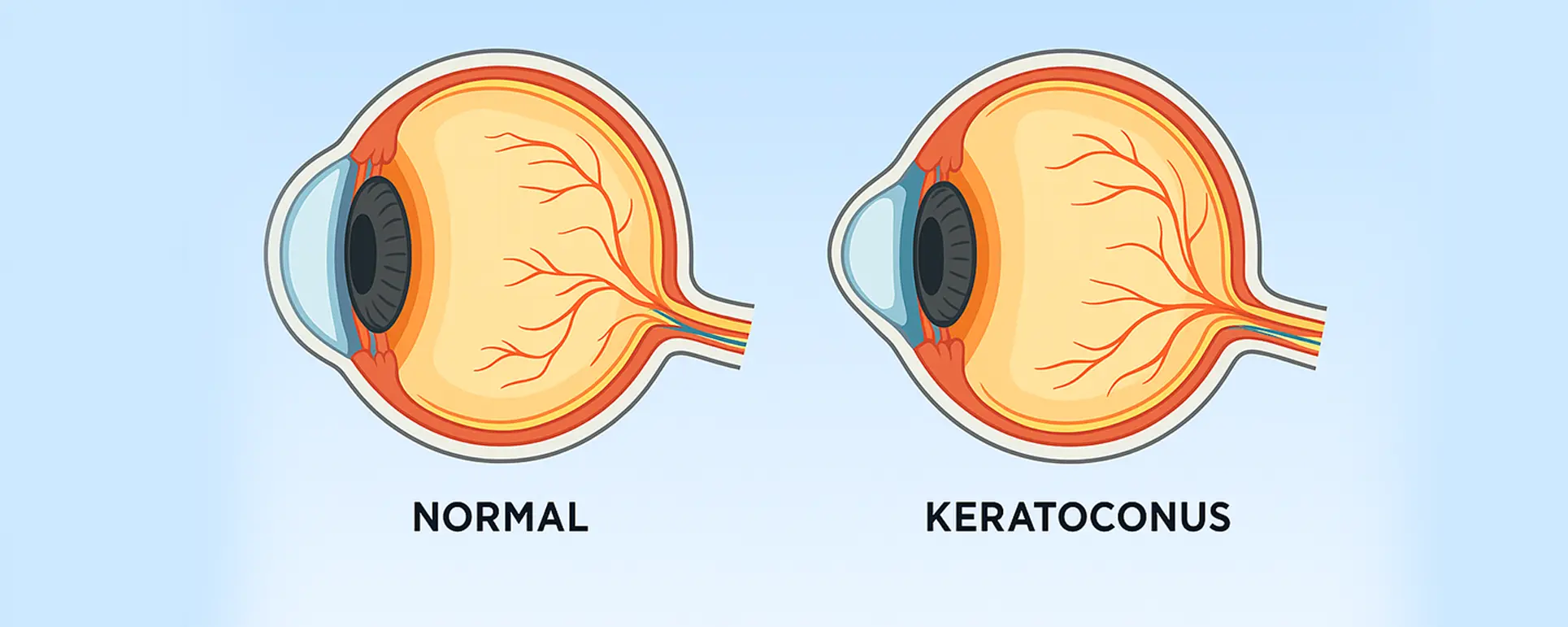
Keratoconus is a progressive eye condition where the cornea—normally dome-shaped—thins and bulges outward into a cone-like shape. This distorts light as it enters the eye, often causing irregular astigmatism and significant visual blur. It typically starts during adolescence or early adulthood and can continue progressing for several years. Early stages might be manageable with glasses or soft contact lenses, but more advanced cases usually require rigid gas permeable lenses, scleral lenses, or surgical options such as corneal cross-linking.
When a keratoconic eye develops a cataract, standard cataract surgery becomes more complicated. The irregular shape of the cornea interferes with accurate measurement of ocular parameters—particularly keratometry and axial length—which are crucial for calculating the correct IOL power. Moreover, visual expectations in keratoconic patients can vary dramatically depending on disease severity, previous treatments, and tolerance to optical imperfections.
Why Refractive Outcomes Are Harder to Predict
One of the main goals of modern cataract surgery is refractive precision. Patients want clear, crisp vision without the need for glasses. That goal becomes more difficult when keratoconus is in the mix. Here’s why:
First, corneal irregularity complicates the very foundation of IOL calculation—accurate biometry. Keratometric readings can be unreliable due to the distorted anterior corneal curvature, and even the most advanced devices can struggle to provide consistent measurements. If the corneal power is underestimated or overestimated, the patient may end up with a significant refractive error post-surgery.
Second, many keratoconus patients have undergone previous interventions—such as cross-linking or intrastromal corneal ring segments (ICRS)—that further change corneal shape and biomechanical properties. These changes can stabilise the disease but introduce even more variability in measurements.
Third, there’s the issue of expectation management. While perfect 6/6 vision might be the benchmark in routine cases, it’s often not realistic in keratoconic eyes, especially in more advanced stages. Instead, success may be defined as a meaningful visual improvement, greater contact lens tolerance, or reduced dependency on rigid lenses.
Assessing the Stage of Keratoconus: A Crucial First Step
Before making any decisions about IOLs or surgical planning, the surgeon needs to evaluate the stage of keratoconus. The approach for mild, stable disease differs significantly from that for advanced, progressive cases.
In mild to moderate keratoconus where the cornea is relatively regular and vision can be corrected well with glasses or soft lenses, a refractive target close to emmetropia may still be achievable. These patients are usually the best candidates for standard IOL power calculation methods, although extra caution is always warranted.
On the other hand, advanced cases with significant scarring, steep K-values, or high irregular astigmatism often require a more conservative approach. In these cases, the goal may shift from achieving spectacle independence to improving functional vision. Some patients may even require combined corneal and cataract procedures, such as deep anterior lamellar keratoplasty (DALK) alongside phacoemulsification.

Choosing the Right IOL: Monofocal vs Toric vs Premium
In most keratoconus patients, monofocal IOLs are the go-to choice. They offer the greatest predictability and least risk of postoperative visual distortion. But even within this category, decisions must be made carefully. Should the lens target slight myopia to allow for better near vision? Or should it aim for a more neutral refractive state, leaving the patient dependent on glasses for near work?
Toric IOLs may be considered in selected cases with stable, regular astigmatism. However, this comes with a word of caution: if the astigmatism is irregular or unstable, the benefits of a toric lens may be negated. Rotational alignment is also critical, and even minor misalignment can significantly reduce the intended correction.
Multifocal and extended depth-of-focus (EDOF) lenses are generally avoided. These lenses split incoming light to provide multiple focal points, which can exacerbate the issues caused by corneal irregularity. The resulting visual artefacts, halos, or reduced contrast sensitivity could outweigh any benefit in patients with keratoconus.
IOL Power Calculation: Navigating Uncertainty
Traditional IOL calculation formulas—like SRK/T, Hoffer Q, or Holladay 1—assume a regular corneal shape. In keratoconic eyes, these assumptions fall apart. This has led to significant interest in finding the best approach for power prediction in such cases.
One common strategy is to use a range of IOL power formulas and look for convergence across different methods. If multiple formulas point to a similar IOL power, confidence in the choice increases. Alternatively, some clinicians prefer to base their decision on the history method, using prior refraction and known corneal changes to reverse-engineer the best estimate.
Advanced formulas like the Barrett Universal II or the Kane keratoconus formula (a recent adaptation of the Kane formula) are showing promise in early studies. These formulas are specifically designed to take the peculiarities of keratoconic eyes into account, improving predictive accuracy.
Role of Corneal Topography and Tomography
Preoperative imaging is a cornerstone of decision-making in keratoconus. Corneal topography maps the anterior surface curvature, helping to identify areas of steepening and asymmetry. Tomography—using technologies like Scheimpflug imaging—goes one step further by also mapping the posterior cornea and providing elevation data.
These images can help differentiate true keratoconus from other conditions that mimic it, such as pellucid marginal degeneration. They can also flag whether the patient has been stable over time or is experiencing progression, which influences surgical timing and refractive planning.
Additionally, topography can help identify candidates for toric IOLs by showing whether the astigmatism is regular enough to be correctable by cylinder power. Surgeons may use these maps to simulate postoperative outcomes and make better-informed decisions.
Managing Irregular Astigmatism
Astigmatism is a near-universal feature in keratoconus, but not all astigmatism is created equal. Regular astigmatism is characterised by a predictable axis and curvature, while irregular astigmatism has skewed axes or multiple peaks. Only regular astigmatism is reliably correctable with toric lenses or spectacles.
In cases of significant irregular astigmatism, patients may still require rigid contact lenses after surgery for optimal visual acuity. Therefore, one of the goals of cataract surgery in these cases may be to improve the baseline corneal clarity and lens transparency so that contact lenses work better postoperatively.
There is also increasing interest in custom IOLs or post-operative light-adjustable lenses (LALs) that can be fine-tuned after implantation. While not yet widely available, they represent a potential breakthrough for difficult refractive cases, including keratoconus.
Special Considerations for Contact Lens Users
Many keratoconus patients rely on rigid gas permeable or scleral contact lenses for visual correction. This poses a unique challenge in the preoperative stage. These lenses temporarily mould the cornea, altering its shape and skewing keratometric readings. If biometry is done while the patient is still wearing these lenses, the results could be wildly inaccurate.

To counter this, surgeons typically recommend a “washout period” during which the patient discontinues contact lens wear to allow the cornea to return to its natural shape. This can vary from several days for soft lenses to several weeks—or even longer—for rigid lenses. Only then can accurate measurements be taken.
However, some patients are so visually dependent on their lenses that going without them for an extended period is not feasible. In such cases, surgeons may need to rely on historical data, average keratometry, or contact lens over-refraction to approximate the corneal power.
Postoperative Expectations and Visual Rehabilitation
After the surgery is done, the journey isn’t over. Keratoconus patients often require a tailored postoperative plan to optimise their final vision. This may involve fitting with new contact lenses, corneal rehabilitation, or, in some cases, additional procedures.
Visual recovery may also take longer. In a regular eye, vision often sharpens within days. In a keratoconic eye, particularly one with advanced irregularity, it may take weeks or even months to reach the best-corrected acuity. That’s why setting realistic expectations before surgery is critical.
In many cases, postoperative spectacles or contact lenses are still required to achieve the best vision. But for many patients, the difference between pre- and post-surgery quality of life is substantial—particularly in terms of clarity, brightness, and overall visual comfort.
Emerging Research and Innovations
The landscape of cataract surgery for keratoconus is evolving. With ongoing advances in IOL technology, biometry, and corneal imaging, the prospects for achieving better refractive outcomes continue to improve.
Research is currently exploring the potential of AI-assisted IOL calculators tailored to keratoconic eyes, as well as wavefront-guided IOLs and light-adjustable technologies. There’s also growing interest in combining cataract surgery with corneal cross-linking in a single procedure, especially for patients at risk of further ectatic progression.
Additionally, clinical trials are looking at how new types of IOL materials and surface designs interact with irregular corneas to maintain visual quality across a range of pupil sizes and lighting conditions.
Frequently Asked Questions (FAQs)
1. Is cataract surgery safe if I have keratoconus?
Yes, cataract surgery can be safely performed in keratoconus patients, but it does require extra care and planning. Keratoconus adds complexity because the shape of the cornea is irregular, which can affect measurements and lens power calculations. That’s why it’s important to work with an ophthalmologist who has experience managing such cases. They’ll use advanced diagnostic tools to ensure the best possible planning and outcomes.
Surgical safety itself is not typically compromised by keratoconus. The techniques used to remove the cataract and implant the intraocular lens are the same as those used in standard cases. However, more caution is applied when interpreting preoperative data and selecting the appropriate type of IOL. Certain techniques may also be adapted depending on the severity of the keratoconus and the presence of corneal scarring or other abnormalities.
It’s also crucial to assess the stability of your keratoconus before surgery. If your condition is still progressing, your surgeon might recommend corneal cross-linking before addressing the cataract. This helps halt further corneal distortion and leads to more predictable surgical planning. In some cases, surgery might even be staged—first to stabilise the cornea, and later to remove the cataract.
In short, yes—cataract surgery is safe, but only if done properly. Make sure to seek out a clinic or surgeon with expertise in both cataract and corneal disorders. The more experienced the surgical team, the better they’ll be at anticipating and managing the unique challenges that come with keratoconus.
2. Can I still get a toric lens if I have keratoconus?
Toric lenses are designed to correct regular astigmatism, which is common in keratoconus. However, the key word here is “regular”. Many keratoconic patients have irregular astigmatism, which cannot be effectively corrected by toric lenses. Whether or not a toric IOL is suitable depends on the stage of your disease and the regularity of your corneal shape, which will be assessed using corneal topography or tomography.
If your keratoconus is mild to moderate and stable, and your corneal astigmatism has a consistent axis, then a toric lens might be a good option. These lenses can significantly reduce your dependence on glasses or contact lenses, especially for distance vision. But accurate alignment is critical—if the toric lens rotates even slightly, it can dramatically reduce its effectiveness. This is why experienced surgical hands are essential.
In more advanced keratoconus, where the astigmatism becomes irregular or the corneal shape unpredictable, a toric lens is typically avoided. In such cases, standard monofocal IOLs are preferred, and astigmatism is managed postoperatively with glasses or specialty contact lenses. Trying to use a toric lens in these scenarios may lead to disappointing outcomes and even more visual distortion.
Ultimately, your surgeon will weigh the risks and benefits of a toric lens carefully. They’ll use mapping technology and a deep understanding of corneal behaviour to decide whether a toric IOL will help or hinder your visual recovery. It’s not a one-size-fits-all answer, and the final decision should be made with full transparency and shared goals.
3. Will I still need glasses or contact lenses after the surgery?
In most keratoconus patients, yes—you will likely still need glasses or contact lenses after cataract surgery. This is because the irregular shape of your cornea often prevents full correction with an intraocular lens alone. While the surgery can dramatically improve the clarity of your vision by removing the cloudy cataract, additional correction is often required for sharp focus.
That said, many patients experience a noticeable improvement in their overall visual function after surgery. Even if glasses or lenses are still needed, you may find them easier to tolerate or more effective than before. Some patients can switch from rigid gas permeable lenses to softer lenses, or reduce their dependency on lenses for certain tasks like driving or reading.
In mild or well-managed keratoconus, it’s sometimes possible to achieve spectacle independence, particularly if a toric IOL is used. But this is the exception rather than the rule. For most, the goal is to enhance the quality of vision and visual potential—not necessarily to eliminate glasses or lenses altogether.
Managing expectations is key. Your surgeon will help you understand the likely outcome based on your eye’s specific characteristics. Even if full independence from corrective lenses isn’t achievable, most patients are still pleased with the level of improvement surgery brings.
4. How accurate are lens power calculations in keratoconic eyes?
Lens power calculations in keratoconus are notoriously tricky. Standard formulas often don’t perform well because they assume the cornea is a regular dome shape—which it isn’t in keratoconus. This leads to potential errors in estimating the eye’s true refractive power, which in turn affects how sharp your vision will be after the new lens is implanted.
To improve accuracy, surgeons may use a combination of formulas and tools to arrive at a more reliable estimate. Devices such as Scheimpflug cameras and optical biometers that measure both the front and back surfaces of the cornea are often used. Some surgeons also apply newer, keratoconus-specific formulas like the Kane keratoconus calculator to improve predictive accuracy.
Another method used is the “historical” approach, which relies on past prescription data and corneal measurements to reverse-engineer the appropriate IOL power. This is particularly useful in patients who’ve had long-standing, stable disease and have built up a reliable track record of measurements. But it still requires a degree of estimation, and the outcome can’t always be guaranteed.
Despite all the tools and formulas available, there is often still a margin of uncertainty. This is why surgeons tend to be conservative with their refractive targets in keratoconic eyes—sometimes aiming for slight myopia rather than trying to hit perfect distance vision. That way, if there’s a refractive surprise, the patient is more likely to end up with usable, functional vision.
5. What happens if my keratoconus gets worse after cataract surgery?
Keratoconus is typically a progressive condition, but it often stabilises with age—especially by the time cataracts are developing. However, there are no guarantees, and in some patients, progression can continue even after cataract surgery. This risk is particularly relevant in younger individuals or those who haven’t had corneal cross-linking.
If progression does occur, it can lead to further visual distortion despite a technically successful cataract surgery. For this reason, surgeons may recommend cross-linking before or even in combination with cataract surgery in certain cases. Cross-linking strengthens the corneal collagen, reducing the risk of further cone development and making refractive outcomes more stable.
If keratoconus worsens after surgery, additional interventions may be necessary. These could include contact lenses, corneal ring implants, or in rare cases, corneal transplant surgery. It’s also possible that your spectacle or lens prescription will need to be adjusted to match the new corneal shape.
That’s why close follow-up after surgery is vital. Ongoing monitoring allows your ophthalmologist to catch any signs of progression early and intervene appropriately. The combination of proactive planning and long-term care gives you the best chance of maintaining good vision over time.

Final Thoughts
Cataract surgery in keratoconus patients is anything but routine. It requires a deeper level of preoperative analysis, careful selection of IOLs, and thoughtful counselling about postoperative expectations. But with the right approach, it’s entirely possible to achieve excellent visual outcomes—even in the most complex cases.
If you or your loved one is facing cataract surgery and also has keratoconus, make sure to consult with a cataract surgeon who has experience in managing these dual diagnoses. And if you’re a clinician, stay updated with the latest tools, techniques, and research—because the standard of care is rapidly advancing.
References
- Kamiya, K., Shimizu, K., Igarashi, A., Matsumura, K. and Komatsu, M., 2015. Clinical outcomes of cataract surgery with toric intraocular lens implantation in eyes with stable keratoconus: a case series. American Journal of Ophthalmology, 160(1), pp.133–139.e1.
Available at: https://doi.org/10.1016/j.ajo.2015.04.001 - Thebpatiphat, N., Hammersmith, K.M., Rapuano, C.J., Ayres, B.D. and Cohen, E.J., 2007. Cataract surgery in keratoconus. Eye & Contact Lens, 33(5), pp.244–246.
Available at: https://pubmed.ncbi.nlm.nih.gov/17873627/ - Watson, M.P., Anand, S., Bhogal, M., Gore, D.M., Moore, J.E. and Coster, D.J., 2014. Cataract surgery outcome in eyes with previous corneal refractive surgery and keratoconus. Journal of Cataract & Refractive Surgery, 40(8), pp.1234–1241.
Available at: https://doi.org/10.1016/j.jcrs.2013.11.037 - Savini, G., Barboni, P. and Hoffer, K.J., 2013. Influence of corneal asphericity on the accuracy of intraocular lens power calculations. Journal of Cataract & Refractive Surgery, 39(11), pp.1709–1715.
Available at: https://pubmed.ncbi.nlm.nih.gov/24160317/ - Kane, J.X., Van Heerden, A., Atik, A. and Petsoglou, C., 2017. Accuracy of 3 intraocular lens power calculation formulas in eyes with keratoconus. Journal of Cataract & Refractive Surgery, 43(6), pp.763–769.