Cataract surgery has come a long way from its early days of rigid, one-size-fits-all lenses. Today, it’s not just about restoring vision—it’s about optimising it. The intraocular lens (IOL) market is evolving fast, with researchers and manufacturers pushing the limits of what’s possible in both material science and optical engineering. Whether you’re a surgeon, a patient considering surgery, or someone simply curious about the future of eye care, this article takes you through the next wave of innovation in IOL design and what it could mean for the quality of your vision.
Why Material Matters in IOL Performance
Let’s start with the basics—material. The stuff your IOL is made from has a significant impact on how it behaves in your eye, both short-term and long-term. It affects everything from optical clarity to the risk of inflammation, glare, or even lens opacification.
Hydrophobic Acrylic: Still the Gold Standard?
Hydrophobic acrylic has been a mainstay in IOL materials for decades, thanks to its stability, biocompatibility, and relatively low rates of posterior capsular opacification (PCO). But it’s not without its flaws. One notorious drawback is the formation of glistenings—tiny fluid-filled microvacuoles that scatter light and reduce contrast sensitivity.
However, not all hydrophobic acrylics are created equal. Recent advances have produced glistening-free hydrophobic acrylics that maintain all the benefits of traditional materials while eliminating one of their key downsides. Clinical studies show significantly better visual clarity and fewer patient complaints of glare or halos with these newer formulations.
Hydrophilic Acrylic: The Underdog?
Hydrophilic acrylic lenses, while less commonly used in some regions, offer greater flexibility during implantation and are less prone to certain types of surface deposits. That said, they tend to have higher rates of PCO. Researchers are now working on hybrid materials that combine the softness and flexibility of hydrophilic acrylics with the low PCO rates of their hydrophobic cousins. These are still largely in development, but early outcomes are promising.
Silicone and PMMA: Phasing Out?
Silicone and polymethylmethacrylate (PMMA) lenses still have a niche in certain clinical scenarios, but their use is on the decline. Silicone lenses can cause complications in patients who may need a vitrectomy later, and PMMA’s rigidity means it requires a larger incision, increasing recovery time. For these reasons, innovation is less focused on these older materials.
Glistening-Free IOLs: A Material Revolution
One of the most talked-about material advancements in recent years is the emergence of glistening-free hydrophobic acrylics. These lenses use advanced polymer formulations to prevent the formation of glistenings altogether, which has massive implications for long-term visual quality.
How Do They Work?
The science behind it involves tighter polymer cross-linking and more homogeneous water content, which reduces the risk of microvacuole formation when the lens equilibrates with aqueous humour. Unlike earlier hydrophobic lenses, which could develop glistenings within months or years, these new lenses remain optically stable over time.
Real-World Impact
Multiple long-term studies have shown that patients with glistening-free IOLs report fewer visual disturbances, particularly in low-light conditions. Surgeons also appreciate their handling properties, as they tend to unfold predictably and centre well in the capsular bag.
The Rise of Enhanced Depth of Focus (EDOF) Lenses
When it comes to optical design, EDOF lenses represent one of the most exciting breakthroughs in recent IOL history. Traditional monofocal lenses only correct for distance, and while multifocal lenses offer multiple focal points, they can come with compromises like halos or reduced contrast sensitivity.
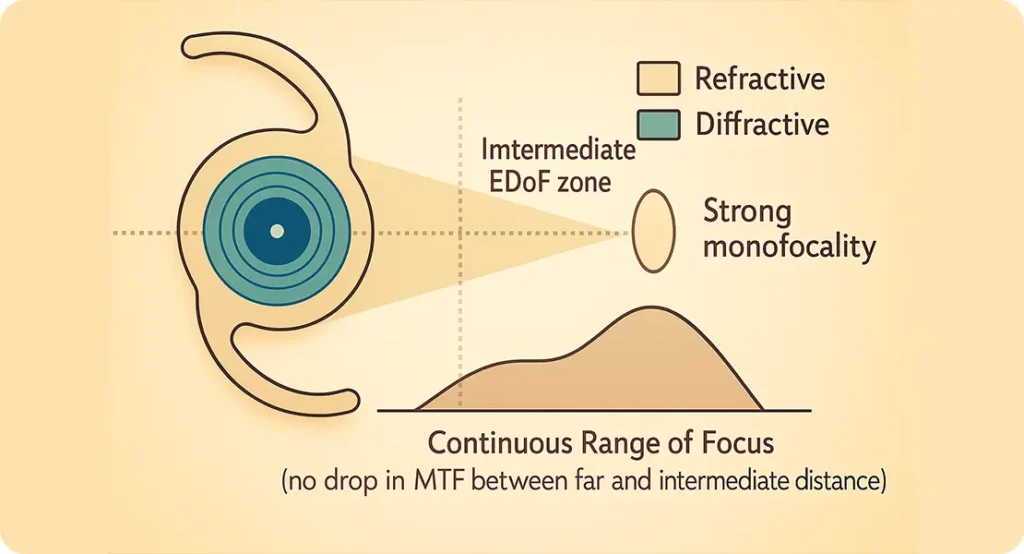
What Sets EDOF Apart?
EDOF lenses work by elongating the focal range rather than creating distinct focal points. This means a smoother transition from near to far vision, with fewer of the side effects associated with multifocals. They’re particularly attractive for patients who want spectacle independence without sacrificing night-time visual clarity.
Optical Engineering Behind EDOF
Most EDOF lenses use proprietary wavefront-shaping or diffractive optics to manipulate how light is focused through the lens. Some also incorporate small aperture technology to increase depth of field. These designs are carefully engineered to reduce chromatic and spherical aberrations, which can otherwise degrade image quality.
Who Benefits Most?
EDOF lenses are particularly useful for active individuals who want to maintain a range of vision without glasses but are sensitive to visual disturbances like halos and glare. They’re also ideal for patients who drive at night or need better intermediate vision for tasks like computer work.
Wavefront-Optimised and Aberration-Neutral Designs
As the field of cataract surgery matures, one of the most exciting developments is the move towards personalised IOL optics. Wavefront-optimised lenses are designed to fine-tune the way light is focused through the eye, based on the individual’s unique corneal profile. Rather than offering a generic lens solution, these advanced IOLs take into account the subtle imperfections—or higher-order aberrations—that exist in the eye’s optical system. By reducing these distortions, patients often report sharper contrast, better clarity, and fewer visual artefacts, especially in challenging lighting conditions like night-time driving.
The technology behind wavefront optimisation relies on highly detailed ocular measurements, often captured via aberrometry. This preoperative imaging captures how light travels through the entire optical pathway, building a custom profile of the eye’s refractive behaviour. The resulting data allows surgeons to choose a lens that doesn’t just correct refractive error but actually enhances the quality of the retinal image. It’s a significant leap from traditional methods, which primarily focus on spherical and cylindrical corrections. As more IOL platforms adopt this approach, patients are increasingly experiencing visual outcomes that more closely resemble their natural, pre-cataract vision.
Aberration Correction vs Neutrality
When it comes to intraocular lens design, there’s a key distinction between lenses that correct aberrations and those that aim to leave the eye’s optics untouched. Aberration-correcting IOLs are particularly useful for eyes that display noticeable imperfections on preoperative scans—such as increased positive spherical aberration. By addressing these specific distortions, the lenses can produce a crisper, more accurate image at the retinal level. This is especially valuable in patients with larger pupils or those who frequently operate in low-light settings, where aberrations can be more pronounced and visually disruptive.
On the other hand, aberration-neutral lenses take a more passive approach. Instead of trying to correct the optical system, they aim to maintain the natural balance of the cornea and internal eye structures. This can be advantageous in patients with near-perfect corneal optics, where introducing corrective elements might actually do more harm than good. In such cases, leaving the natural optical profile untouched may yield better outcomes. The decision between correction and neutrality often comes down to a detailed analysis of the patient’s visual needs, ocular anatomy, and lifestyle demands.
The Role of Wavefront Technology
Wavefront technology is a major contributor to the ongoing refinement of cataract surgery. It works by measuring how light waves travel through the eye and identifying any deviations or distortions in their path. This process doesn’t just look at basic refractive errors—it captures a comprehensive map of both lower- and higher-order aberrations that could affect visual quality. These measurements allow for a much more personalised approach when selecting IOLs, and are particularly helpful in borderline or complex cases where conventional methods fall short.

As wavefront-guided planning becomes more integrated into cataract surgery workflows, we’re starting to see a shift towards data-driven decisions in lens selection. Some IOL systems even incorporate preoperative wavefront measurements into their lens design algorithms, tailoring the optics to enhance contrast sensitivity or reduce light scatter. This personalisation doesn’t just help with the initial surgical outcome—it can also reduce the need for post-operative fine-tuning or additional procedures. As the technology evolves, we may see wavefront data playing a role not only in lens selection but in intraoperative alignment and long-term visual tracking.
Blue Light Filtering: An Ongoing Debate
The incorporation of blue light filtering in IOLs has sparked both interest and debate in ophthalmology circles. These lenses are tinted to absorb short-wavelength blue light, which is thought to contribute to oxidative stress in the retina—potentially increasing the risk of conditions like age-related macular degeneration (AMD). Advocates for blue light filters argue that they mimic the natural yellowing of the ageing crystalline lens and can provide a layer of protection that would otherwise be lost after cataract removal. Some patients also report reduced glare sensitivity and improved comfort in bright environments.
However, the flip side of the argument raises important concerns. Blue light is not entirely harmful—it plays a key role in regulating the circadian rhythm, helping maintain a healthy sleep-wake cycle. Over-filtering could impair this natural process, potentially leading to sleep disturbances or mood shifts in sensitive individuals. There is also the question of reduced scotopic vision, where blocking blue light may affect vision in dim settings. As such, the evidence remains inconclusive, and most ophthalmologists treat blue-light filtering as a personal or situational preference rather than a clinical necessity for all patients.
Pros and Cons
The potential benefits of blue-light filtering IOLs are certainly appealing to many patients and clinicians. For individuals with a family history of macular degeneration or signs of retinal vulnerability, these lenses offer a theoretical layer of defence. They can also improve visual comfort in high-glare settings, such as driving on sunny days or working under fluorescent lighting. Some users even claim better visual endurance during screen-heavy tasks, which is becoming more relevant in today’s digital world.
Yet, it’s equally important to consider the limitations. Not all patients respond well to the yellow tint, and some may find it alters colour perception slightly—particularly in artistic or design-related work. Others may not feel any tangible benefit at all. Clinical trials have yet to reach consensus on whether these lenses provide significant long-term protection against retinal damage. In the absence of conclusive evidence, blue-light filtering IOLs remain an option best reserved for carefully selected cases, rather than a default choice for every cataract patient.
What’s the Future?
Looking ahead, innovation in light filtering is likely to focus on personalisation and adaptability. Rather than static filters embedded within the lens, future designs may allow dynamic modulation—altering their properties based on ambient light or time of day. Smart chromophores or electrochromic technologies, similar to transition lenses in glasses, are being explored as potential ways to achieve this. These would offer the best of both worlds: protecting the retina from harmful rays during peak exposure, while allowing essential wavelengths through when needed.
In the meantime, the trend is moving toward selective filtering. Some research is exploring the use of filters that block only the most harmful high-energy visible (HEV) blue light while preserving the wavelengths essential for biological rhythms and colour vision. Such precision filtering could offer a more balanced approach, addressing both safety and functionality. As research continues and long-term data accumulates, we’ll likely gain a clearer picture of which patients stand to benefit most—and under what circumstances blue light filtering should be recommended.
Injectable and Shape-Changing IOLs
Looking even further ahead, injectable and shape-changing IOLs are being developed to mimic the accommodative power of the natural lens. These are not widely available yet, but they represent an exciting frontier.
How They Work
Injectable lenses are inserted in a fluid or gel state and solidify in the capsular bag, conforming to its shape. Some experimental designs even include light-adjustable polymers or electroactive materials that can change shape in response to stimuli.
The Goal: True Accommodation
The holy grail of IOL design is a lens that can change focus dynamically, just like a natural lens. While several accommodating lenses have hit the market in the past, most have failed to deliver consistent results. With new materials and smarter designs, we’re inching closer to making this dream a reality.
Preloaded and Smart Delivery Systems
Another area of innovation lies not in the lens itself, but how it’s delivered. Preloaded IOL systems are now standard in many clinics, improving sterility and surgical efficiency. The future may bring robotic injectors and AI-assisted alignment tools.
Precision Matters
Many premium lenses require exact centration and orientation to work properly—especially toric or EDOF lenses. Smart delivery systems using real-time eye tracking and intraoperative aberrometry can help surgeons achieve pinpoint accuracy.
Sustainability and Biodegradable Options
As cataract surgery volumes rise globally, attention is turning to environmental impact. Research is underway on biodegradable materials and fully recyclable packaging for IOLs and their delivery systems.

Green Surgery?
It’s early days, but with climate concerns rising, don’t be surprised if the next generation of IOLs comes with a green certification. Manufacturers are already exploring how to reduce single-use plastics and carbon emissions during production.
AI and Personalised IOL Selection
Artificial intelligence is playing a growing role in helping surgeons select the right IOL for each patient. Algorithms trained on thousands of outcomes can now recommend the most suitable lens type, power, and design based on your biometric data and lifestyle needs.
A Tailored Experience
Rather than relying solely on surgeon judgement or patient preference, these tools use predictive modelling to optimise visual outcomes. This can be particularly helpful in borderline cases or when patients have unusual ocular anatomy.
Final Thoughts: The Future Is Clearer Than Ever
So, what’s next in cataract surgery? If current trends continue, we’re moving towards a future where IOLs are no longer just passive replacements for your clouded lens—but active participants in vision enhancement. With better materials, smarter designs, and even AI-assisted selection, the entire process is becoming more precise, more personalised, and more powerful.
Whether you’re a surgeon looking to stay ahead of the curve or a patient planning your own procedure, the bottom line is this: the era of one-size-fits-all cataract surgery is coming to a close. The future is bespoke, biocompatible, and brilliantly clear. If you are considering cataract surgery and would like to learn more, then feel free to contact us at the London Cataract Centre for a consultation with one of our expert cataract surgeons.
References
- Werner, L. (2020) ‘Intraocular lens materials and design: Past, present, and future’, Eye, 34(1), pp. 29–41.
- Auffarth, G.U., Yildirim, T.M. and Khoramnia, R. (2021) ‘Glistening-free hydrophobic acrylic intraocular lenses: A new benchmark?’, Journal of Cataract & Refractive Surgery, 47(3), pp. 295–302. Available at: https://journals.lww.com/jcrs/Fulltext/2021/03000/Glistening_free_hydrophobic_acrylic_intraocular.3.aspx
- Kohnen, T. and Suryakumar, R. (2022) ‘Enhanced depth of focus intraocular lenses: Principles, outcomes, and future directions’, American Journal of Ophthalmology, 237, pp. 208–217.
- Kollbaum, P.S., Jansen, M.E. and Thibos, L.N. (2018) ‘Optical performance of presbyopia-correcting intraocular lenses’, Journal of Refractive Surgery, 34(8), pp. 507–518.
- Rocha, K.M., Soriano, E.S. and Chalita, M.R. (2019) ‘Wavefront technology in cataract surgery: Aberration-based IOL selection and outcomes’, Current Opinion in Ophthalmology, 30(1), pp. 32–38. Available at: https://journals.lww.com/co-ophthalmology/Fulltext/2019/01000/Wavefront_technology_in_cataract_surgery_.6.aspx

