If you have been diagnosed with glaucoma and are now being advised to consider cataract surgery, it is completely natural to feel uncertain about lens choices. Many patients worry that having glaucoma automatically rules out certain lenses, especially premium options they may have heard about. At the same time, you may be concerned about making a decision that could affect your long-term vision.
Cataract surgery is not just about removing a cloudy lens. The type of artificial lens placed in your eye plays a major role in how you see afterward. When glaucoma is part of the picture, that decision becomes more nuanced rather than more limited.
In this article, we explain how glaucoma influences cataract lens selection in a clear, step-by-step way. We look at why glaucoma severity matters, how contrast sensitivity and visual fields are affected, and why some lenses are safer and more suitable than others. Our aim is to help you understand the reasoning behind lens recommendations so you can feel confident, not restricted.
Understanding Why Lens Choice Matters More in Glaucoma
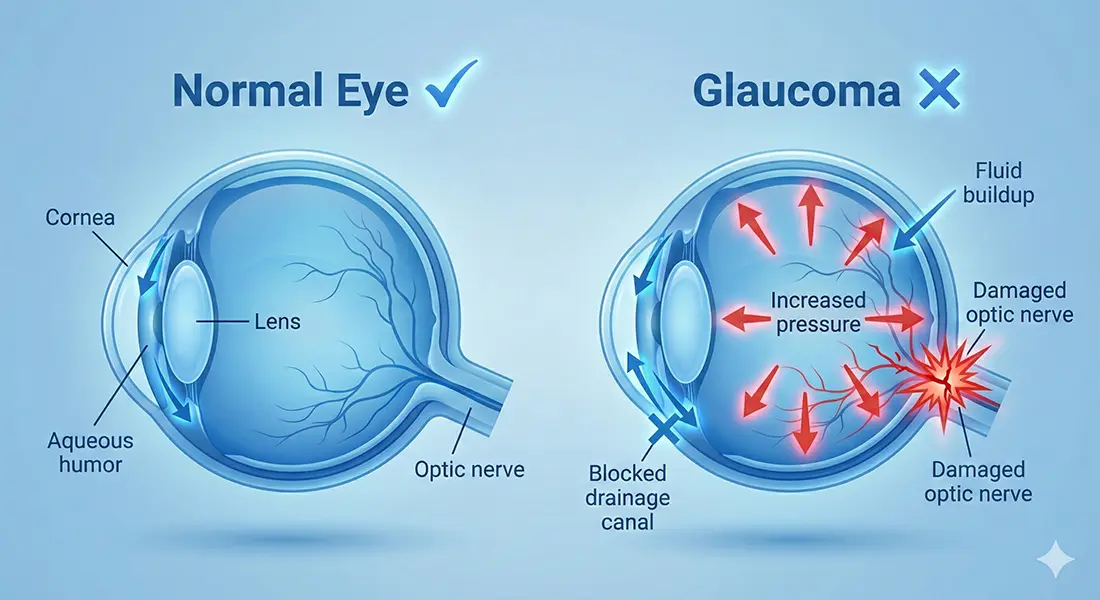
Glaucoma affects the optic nerve, which is responsible for transmitting visual information from the eye to the brain. Damage to this nerve can reduce peripheral vision and contrast sensitivity, even when central vision still seems good. These changes influence how different lenses perform in real-world conditions.
Not all cataract lenses interact with vision in the same way. Some lenses prioritise sharpness at one distance, while others split or stretch light to provide vision at multiple distances. In a healthy eye, this may work well, but in an eye affected by glaucoma, the same optical design can behave differently.
This is why lens choice is not just about preference in glaucoma patients. It is about protecting functional vision and avoiding unnecessary compromises.
A Quick Overview of Glaucoma and Vision
Glaucoma is often described as a condition that affects side vision first. While this is broadly true, the reality is more complex. Many patients experience subtle changes in contrast, clarity, and visual confidence long before severe field loss occurs. Contrast sensitivity refers to how well you can distinguish objects from their background, especially in low light or foggy conditions. Glaucoma can reduce this sensitivity, making vision feel less crisp even if acuity tests look acceptable. Understanding these visual changes helps explain why some lenses are recommended cautiously in glaucoma patients.
Why Cataract Surgery Is Still Beneficial in Glaucoma

Having glaucoma often raises understandable concerns about eye surgery. However, glaucoma does not automatically make cataract surgery unsafe or ineffective. In many cases, removing a cataract can significantly improve how well you see and function day to day.
Here’s why cataract surgery can still be beneficial:
1. Glaucoma Does Not Exclude Cataract Surgery – The presence of glaucoma alone does not mean cataract surgery should be avoided. With proper planning, many patients with glaucoma undergo surgery safely and successfully.
2. Vision Quality Often Improves – Removing the cloudy lens allows more light to enter the eye. This can improve brightness, contrast, and colour perception, even when some vision loss from glaucoma is present.
3. Eye Pressure May Improve in Some Cases – Cataract surgery can sometimes help lower eye pressure slightly. While it is not a treatment for glaucoma itself, this pressure benefit can be helpful for some patients.
4. Daily Function and Confidence Often Increase – Clearer vision can make everyday tasks such as reading, walking, and driving easier. Many patients report feeling more confident and visually comfortable after surgery.
The key difference with glaucoma is not whether cataract surgery should be done, but how carefully it is planned. By tailoring the approach to your eye health, we can protect remaining vision while helping you gain meaningful visual improvement and better quality of life.
How Glaucoma Severity Influences Lens Decisions
The stage of glaucoma is one of the most important factors in lens selection. Early, stable glaucoma is very different from advanced disease with significant field loss. In early glaucoma, central vision and contrast may still be relatively well preserved. This allows more flexibility in lens choice, although caution is still required. In moderate to advanced glaucoma, preserving contrast and visual clarity becomes the priority. Lens options are chosen more conservatively to avoid further functional loss.
Visual Field Loss and Its Practical Impact
Visual field loss means that certain areas of your vision are missing, most often at the edges. You may not notice this all the time, but it can affect how you move through space, detect motion, and feel confident in everyday situations. These changes can subtly influence daily life.
Lenses that reduce image contrast or create optical artefacts can make these difficulties more noticeable. We take this seriously because added visual disturbance can increase strain and reduce comfort. This is why visual field status is always considered before recommending any lens option.
Our goal is to support the vision you already have, not add new visual stress. We focus on preserving clarity, comfort, and confidence in real-world situations. Careful lens selection helps ensure your vision feels as natural and usable as possible.
Contrast Sensitivity: A Key Factor in Lens Safety
When you’re living with glaucoma, vision quality is about more than sharpness on a chart. Contrast sensitivity plays a major role in how safely and comfortably you function day to day, especially in low light or poor weather. Subtle reductions in contrast can feel far more noticeable in eyes already affected by glaucoma.
Contrast sensitivity matters in lens selection because:
- It affects real-world vision – Seeing edges, steps, kerbs, and obstacles clearly in low light is essential for everyday safety and confidence.
- Some premium lenses reduce contrast slightly – This is a trade-off for providing multiple focal points, which may be insignificant in healthy eyes.
- Glaucoma amplifies small changes – In glaucoma, even mild contrast reduction can become more noticeable and affect visual comfort.
- Lens choice must be individualised – Premium lenses are not automatically unsafe, but they need careful selection based on your visual needs and disease status.
By prioritising contrast sensitivity alongside sharpness, we can choose lenses that support both visual performance and long-term safety.
Monofocal Lenses: The Safest Baseline Option
Monofocal lenses provide clear vision at a single distance, most commonly set for distance vision. We value these lenses because they do not split light or significantly reduce contrast. This makes vision more predictable and stable.
For many people with glaucoma, monofocal lenses are the safest and most reliable option. We know they preserve contrast sensitivity and perform consistently across different lighting conditions. This reliability is especially important when visual reserve is already reduced.
While you will usually need glasses for reading, many patients appreciate the clarity and confidence monofocal lenses provide. We focus on supporting comfortable, dependable vision rather than chasing spectacle independence. For many, visual stability matters most.
Why Monofocal Lenses Are Often Recommended First
When glaucoma is part of the picture, lens choice becomes especially important. Our priority shifts towards protecting visual quality and keeping demands on the visual system as low as possible. This is why monofocal lenses are often recommended as the starting point.
Here’s why monofocal lenses are usually favoured:
1. They Work With the Eye’s Natural Optics – Monofocal lenses provide clear vision at a single focal point without splitting light. This allows the eye to work in a more natural and predictable way.
2. They Place Minimal Demand on the Visual System – Because monofocal lenses don’t rely on complex optics, they are gentler on the visual system. This is particularly important when the optic nerve is already under strain from glaucoma.
3. Clarity and Contrast Are Prioritised – In glaucoma, preserving contrast sensitivity often matters more than reducing dependence on glasses. Monofocal lenses support sharp, high-quality vision with fewer visual compromises.
4. They Offer Predictable and Stable Outcomes – Monofocal lenses have a long track record and deliver consistent results. This reliability makes them a safe and sensible default choice for many patients.
For patients with glaucoma, the goal is not just clearer vision, but comfortable and dependable vision. Monofocal lenses help us achieve this by prioritising clarity and contrast over complexity. That’s why we often recommend them first, unless there’s a clear reason to explore other options together.
Toric Lenses and Glaucoma
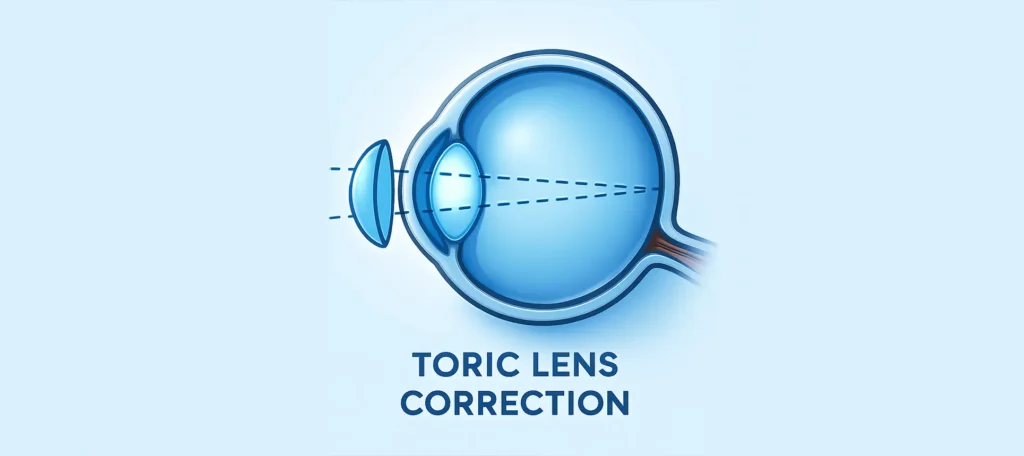
Toric lenses are designed to correct astigmatism and improve visual clarity. We like these lenses because they do not split light or reduce contrast in the way multifocal lenses can. This makes them more predictable for everyday vision.
For people with glaucoma who also have astigmatism, toric monofocal lenses can be an excellent option. We see them improve sharpness and reduce blur without introducing additional optical compromises. This balance is important when protecting remaining visual function.
As long as the eye is otherwise suitable, toric lenses are generally considered safe in glaucoma. We assess eye health carefully to ensure stability and proper alignment. When chosen appropriately, toric lenses can enhance clarity while maintaining visual comfort and confidence.
Multifocal Lenses: Why Caution Is Needed
Multifocal lenses work by dividing light into different focal points for distance and near vision. This design can reduce contrast and introduce glare or halos.
In glaucoma patients, reduced contrast sensitivity means these effects may feel more pronounced. Visual field loss can further amplify discomfort or dissatisfaction.
For this reason, multifocal lenses are usually approached cautiously or avoided in moderate to advanced glaucoma.
Extended Depth-of-Focus Lenses and Glaucoma
Extended depth-of-focus (EDOF) lenses are designed to improve range of vision by stretching focus rather than splitting light into multiple focal points. This approach can reduce some of the visual side effects seen with traditional multifocal lenses. However, when glaucoma is present, careful selection and realistic expectations are essential.
EDOF lenses may be considered in glaucoma because:
- They preserve contrast better than multifocal lenses – By avoiding sharp light splitting, EDOF lenses tend to have fewer issues with glare and contrast loss.
- Suitability depends on disease stage – In very early, stable glaucoma, these lenses may be considered cautiously after thorough assessment.
- Expectations must be realistic – Vision gains are often more subtle, and reading glasses may still be needed in some situations.
- Careful assessment is essential – Not everyone with glaucoma is suitable, and contrast preservation always remains the priority.
By assessing your eye health carefully and discussing trade-offs openly, we can decide whether an EDOF lens is a safe and sensible option for you.
Why “Premium” Does Not Always Mean “Better”
The term “premium lens” can be misleading. It often suggests superior quality, but when glaucoma is present, the safest option is not always the most advanced one. We focus on what protects your vision, not what sounds impressive.
Premium lenses are designed for convenience, such as reducing dependence on glasses, rather than supporting a vulnerable optic nerve. In some cases, added optical complexity can reduce contrast or increase visual strain. We often find that simpler designs provide better long-term comfort.
Understanding this helps shift the decision in a healthier direction. Instead of asking what you might be missing out on, we encourage you to ask what best preserves the vision you have. This perspective supports confidence and protects visual quality over time.
The Importance of Individual Assessment
No two people with glaucoma experience the condition in exactly the same way. Vision needs, disease behaviour, and daily demands vary widely from person to person. This is why individual assessment is far more valuable than applying broad rules or assumptions.
Individual assessment matters because:
- Disease severity and stability differ – Early, stable glaucoma presents very different considerations compared with more advanced or progressing disease.
- Lifestyle and visual priorities vary – Your work, hobbies, night driving needs, and reading habits all influence what is safe and practical for you.
- Safety must be balanced with function – A personalised review allows us to weigh visual benefits against potential risks thoughtfully.
- Generic rules are rarely helpful – Lens recommendations should be based on your specific eyes, not on marketing labels or blanket exclusions.
By focusing on your individual eye health and visual goals, we can recommend options that are safer, more realistic, and better suited to your long-term needs.
Lifestyle Considerations in Glaucoma Patients
How you use your vision in daily life matters greatly. Activities like night driving, moving through uneven lighting, or navigating busy environments place higher demands on contrast sensitivity and depth perception. We always consider these real-world needs, not just clinical measurements.
If your lifestyle involves visually challenging situations, lens choices should prioritise clarity and confidence rather than theoretical convenience. We aim to support stable, comfortable vision that performs well in everyday conditions. This helps reduce strain and uncertainty.
Open discussion about your daily activities is essential. When you share how and where you rely on your vision most, we can guide safer, more appropriate decisions. Matching lens choice to lifestyle protects both visual function and confidence.
Glaucoma Progression and Future Vision
Glaucoma is a chronic condition and may progress over time, even when treatment is well managed. We always consider this long-term reality when discussing lens choices. Decisions made today need to support your vision for years to come.
A lens that feels acceptable now may become less comfortable if contrast sensitivity declines in the future. We see this especially with more complex lens designs. Conservative options often provide greater visual stability as the disease evolves.
Thinking ahead is an essential part of responsible planning. We focus on protecting visual function rather than chasing short-term convenience. This forward-looking approach helps maintain comfort and confidence over time.
Combined Glaucoma and Cataract Surgery Considerations
When cataract and glaucoma surgery are performed together, planning becomes more nuanced. We need to manage eye pressure while also delivering reliable visual outcomes. This makes lens choice and surgical strategy especially important.
Combined procedures require careful consideration because:
- Vision reliability is critical during pressure management – Clear, predictable vision supports safety and confidence while glaucoma treatment is optimised.
- Monofocal lenses are often preferred – They offer stability and predictability, which is valuable when multiple surgical goals are being addressed at once.
- Contrast preservation remains a priority – Maintaining functional vision is more important than maximising range in eyes affected by glaucoma.
- The plan is fully individualised – We tailor the surgical approach to protect both long-term vision and overall eye health.
By aligning lens choice with glaucoma management, we aim to achieve outcomes that are safe, stable, and appropriate for your specific eye condition.
Common Misconceptions About Glaucoma and Lens Choice
One common misconception is that glaucoma automatically rules out all premium lenses. We know the reality is more nuanced, and suitability depends on disease stage, visual function, and individual needs rather than labels alone.
Another misunderstanding is that choosing a simpler lens means accepting inferior outcomes. In glaucoma, simpler lens designs often preserve contrast and provide better functional vision. We frequently see patients do better with stability than complexity.
Clear explanation helps dispel these myths. When you understand why certain options are recommended, decisions feel more reassuring and informed. We focus on what best protects your vision, not on assumptions or marketing terms.
Asking the Right Questions Before Choosing a Lens
Before choosing a lens, it’s important to look beyond marketing language and focus on how the lens will actually perform in daily life. For people with glaucoma, small differences in contrast or glare can have a meaningful impact over time. Clear discussion helps you make a decision that feels informed rather than rushed.
The right questions to ask include:
- How does this lens affect contrast and glare? – Understanding real-world vision in low light or challenging conditions is more important than headline features.
- What are the trade-offs involved? – Every lens design involves compromises, and knowing them upfront helps avoid disappointment later.
- How does my stage of glaucoma influence suitability? – Early, stable disease is very different from more advanced glaucoma when it comes to lens choice.
- Which option best protects long-term vision? – The safest choice is often the one that preserves reliable vision over time, not the most complex design.
By asking thoughtful questions and understanding the reasoning behind recommendations, you can make lens decisions based on clarity and confidence rather than pressure.
Top of Form
Bottom of Form
The Role of Specialist Guidance
Lens selection in glaucoma requires experience and careful clinical judgement. We look at both conditions together, not in isolation, so decisions are made with a full understanding of current vision and future risk. This specialist approach reduces uncertainty and protects visual function.
At London Cataract Centre, we guide glaucoma patients through cataract surgery and lens choices with a strong focus on safety, contrast preservation, and long-term visual stability. We take time to explain why certain options are recommended and how they support everyday vision.
This approach helps you feel reassured rather than limited. Instead of focusing on what you cannot have, we focus on what best protects your sight. Clear guidance builds confidence and supports better outcomes over time.
Balancing Safety and Expectations
It’s completely natural to want the best possible outcome from cataract surgery. When glaucoma is present, we define “best” as protecting the vision you rely on and maintaining confidence in daily life. Safety and function take priority over novelty.
Sometimes this means prioritising visual stability over complete spectacle independence. We know that understanding this balance helps align expectations with what the eye can comfortably support. Choosing stability often leads to more dependable, stress-free vision.
When expectations are realistic, satisfaction is usually higher. We focus on helping you feel informed and confident in your decisions. Clear understanding allows outcomes to feel reassuring rather than disappointing.
FAQs:
1. Does having glaucoma automatically limit my cataract lens options?
Glaucoma does not automatically exclude you from choosing certain cataract lenses. What matters most is the stage and stability of your glaucoma, along with how your vision is currently functioning. Lens choice is guided by protecting contrast and functional vision rather than applying blanket restrictions.
2. Why is lens choice more important when glaucoma is present?
Glaucoma affects the optic nerve, which plays a key role in contrast sensitivity and visual confidence. Some lens designs can reduce contrast or introduce visual artefacts that feel more noticeable in glaucoma. Careful lens selection helps preserve usable, comfortable vision in everyday situations.
3. Are monofocal lenses the safest option for people with glaucoma?
Monofocal lenses are often recommended because they provide clear vision at one distance without splitting light. This preserves contrast sensitivity and creates predictable visual outcomes. For many glaucoma patients, this reliability supports better long-term comfort and confidence.
4. Can toric lenses be used safely if I have glaucoma and astigmatism?
Toric lenses are generally considered safe for glaucoma patients when astigmatism is present. They improve clarity by correcting corneal shape without reducing contrast. As long as the eye is stable, toric monofocal lenses can enhance vision without adding unnecessary optical complexity.
5. Why are multifocal lenses usually avoided in glaucoma patients?
Multifocal lenses divide incoming light to provide vision at multiple distances, which can reduce contrast sensitivity. In eyes affected by glaucoma, this reduction may feel more pronounced and lead to glare or visual discomfort. This is why they are usually avoided, especially in moderate or advanced disease.
6. Are extended depth-of-focus lenses ever suitable in glaucoma?
In very early and stable glaucoma, extended depth-of-focus lenses may sometimes be considered. These lenses stretch focus rather than splitting light, which helps preserve contrast better than multifocal designs. Careful assessment and realistic expectations are essential before considering this option.
7. How does contrast sensitivity influence lens recommendations?
Contrast sensitivity affects how well you see in low light, poor weather, or busy environments. Glaucoma often reduces this ability, even when vision seems sharp on testing. Lens choices aim to protect contrast so everyday vision remains safe and comfortable.
8. Will cataract surgery still improve my vision if I have glaucoma?
Yes, cataract surgery often improves brightness, clarity, and overall visual comfort in people with glaucoma. While it does not reverse optic nerve damage, removing a cloudy lens can make better use of remaining vision. Many patients notice meaningful functional improvement after surgery.
9. Should future glaucoma progression affect my lens decision today?
Yes, future disease progression is an important consideration. A lens that feels acceptable now may become less comfortable if contrast sensitivity declines over time. Conservative lens choices often provide greater visual stability as glaucoma evolves.
10. How do specialists decide which lens is right for a glaucoma patient?
Specialists assess glaucoma severity, visual fields, contrast sensitivity, lifestyle needs, and long-term risk. The goal is to balance clarity, comfort, and safety rather than focusing on convenience alone. This personalised approach helps protect vision while supporting daily confidence.
Final Thoughts: Making Safe, Informed Lens Choices With Glaucoma
Glaucoma does not automatically restrict your cataract lens options, but it does change how those options should be evaluated. The safest choices prioritise contrast sensitivity, visual stability, and long-term comfort rather than spectacle independence alone. By understanding how Glaucoma affects functional vision and how different lenses interact with it, you can make decisions that protect the sight you rely on every day. Careful, individual assessment is far more important than labels or assumptions.
If you’re thinking about Glaucoma treatment in London, you can get in touch with us at London Cataract Centre to discuss your options in detail and ensure your cataract surgery plan supports both your current vision and long-term eye health.
References:
1. Central contrast sensitivity as an outcome measure in randomized controlled trials in glaucoma a systematic review, Life, 15(7), 1043. https://www.mdpi.com/2075-1729/15/7/1043
2. Comparison of the visual outcomes of enhanced and standard monofocal intraocular lens implantations in eyes with early glaucoma, Journal of Clinical Medicine, 12(18), 5830. https://www.mdpi.com/2077-0383/12/18/5830
3. Reviews specific considerations around IOL selection for glaucoma, including contrast sensitivity impacts. https://pubmed.ncbi.nlm.nih.gov/21507514/
4. Effects of blue-light-filtering intraocular lenses on contrast sensitivity in patients with glaucoma, Medicine (Baltimore), e36821. https://pmc.ncbi.nlm.nih.gov/articles/PMC10754553/ 5. Evaluates functional factors including contrast sensitivity and visual field considerations for premium IOLs in glaucoma patients. https://pubmed.ncbi.nlm.nih.gov/37760095/