If you’ve had cataract surgery and you’re now noticing floaters drifting across your vision, you’re far from alone. In fact, clearer vision often reveals floaters that were there all along. That can be unsettling—especially when you’ve just gone through surgery to make your sight better, not more distracting. In this guide, I’ll talk to you directly about what floaters are, why they can become more obvious after your lens is replaced, which symptoms are simply part of normal healing, and the specific situations where you should get urgent help. We’ll also walk through the full menu of treatments—from the “do nothing yet” approach (which is often the right first step) to laser options and vitrectomy—so you can understand what’s available and how decisions are made.
My goal is simple: give you a plain-English, practical playbook so you know what’s normal, what isn’t, and what to do next.
Key points at a glance
- Floaters are common and usually result from tiny clumps in the vitreous gel casting shadows on your retina.
- After cataract surgery, floaters often feel more noticeable because your visual system is getting brighter, higher-contrast images through a clear lens.
- Most floaters are harmless, but a sudden storm of new floaters, flashes of light, or a “curtain” over part of your vision can signal a retinal tear or detachment and needs urgent assessment.
- Monitoring is usually the first step. Many floaters fade from your awareness over weeks to months.
- Treatments exist—including YAG vitreolysis for selected floater types and vitrectomy for severe, persistent symptoms—but they’re used thoughtfully because all procedures carry risks.
- Special situations such as high myopia, a recent YAG capsulotomy, or vitreous complications can alter risk and management.
First things first: what are floaters?

Floaters are little opacities inside the clear jelly that fills the back of the eye—the vitreous. Think of the vitreous as a transparent gel scaffold. With time, and sometimes after surgery, that gel becomes more watery and its fine collagen fibres clump together. These clumps cast tiny, moving shadows on the retina, which your brain interprets as specks, threads, blobs, or ring-shaped wisps that drift when you move your eye and then “lag” behind a moment.
One common type, the Weiss ring, looks like a doughnut or loop and typically appears when the vitreous separates from the optic nerve head during a posterior vitreous detachment (PVD). PVD is very common with age. Most of the time, it’s benign. Sometimes, though, as the vitreous peels away it tugs on the retina; if the retina tears, that’s an emergency.
Why floaters can seem worse after cataract surgery
You may wonder: “Did my operation cause these floaters?” In most cases, no. Cataract surgery replaces the cloudy natural lens with a clear artificial one. That clarity increases retinal illumination and contrast, which makes pre-existing floaters more visible. Put simply, the world (and the shadows) now looks sharper and brighter.
Other reasons floaters get your attention after surgery include:
- Your brain is re-calibrating. After months or years of haze from the cataract, your visual system suddenly receives crisp images. Background artefacts—like floaters—stand out.
- Dilated pupils and bright clinic lights can accentuate floater visibility in the early postoperative period.
- True changes in the vitreous sometimes occur around the time of surgery. Cataract surgery can be associated with vitreous shifts, and in the weeks afterwards some people experience a PVD, which can introduce new floaters.
- Lens optics can change perception. Certain implant designs, such as multifocal or EDOF lenses, alter contrast in ways that may make some people more aware of existing vitreous opacities compared with a standard monofocal.
What’s normal, and what’s not?

Likely normal:
- A few specks or strands drifting in and out of view, most obvious against plain bright backgrounds such as a blue sky or white screen.
- Gradual reduction in awareness over weeks as your brain adapts and as post-op inflammation settles.
- Intermittent, mild awareness that doesn’t interfere with reading, driving, or daily life.
Not normal—seek urgent assessment:
- A sudden shower of new floaters that appear over hours to a day.
- Flashes of light, particularly in dim light, like a camera flash in the periphery.
- A curtain, veil, or shadow encroaching from the edge of your vision.
- Blurred or distorted central vision that doesn’t improve by blinking and isn’t explained by your immediate post-op course.
- Any decrease in vision that is rapid or progressive.
A typical timeline after surgery
Everyone heals at their own pace, but here’s a reasonable arc:
- Days 1–7: Vision brightens and sharpens. Floaters can feel prominent, partly because you’re paying close attention to your new vision.
- Weeks 2–6: Awareness of mild floaters often starts to fade. If a PVD occurs, it most often happens around this window, and you could notice a new ring-shaped floater or a flurry of specks. That’s the moment to contact your clinic.
- Months 2–6: Many people report that floaters are less intrusive—either they’ve drifted out of the central visual axis, become less optically dense, or your brain has learned to ignore them.
- After a YAG capsulotomy: Some people notice temporary new floaters from capsule debris; these generally settle, though the same red-flag rules apply.
What else can look like floaters?
Not every speck is a classic vitreous floater. Your clinician will consider:
- Residual surgical bubbles from viscoelastic or irrigating solutions.
- Inflammatory cells or pigment in the vitreous.
- Tiny blood spots in the vitreous (vitreous haemorrhage).
- Lens material remnants in cases of posterior capsular rupture.
- Posterior capsule opacification, which is not a floater but a film on the membrane behind your lens implant.
- Dry eye or tear-film debris, which moves with blinks, not with eye movements.
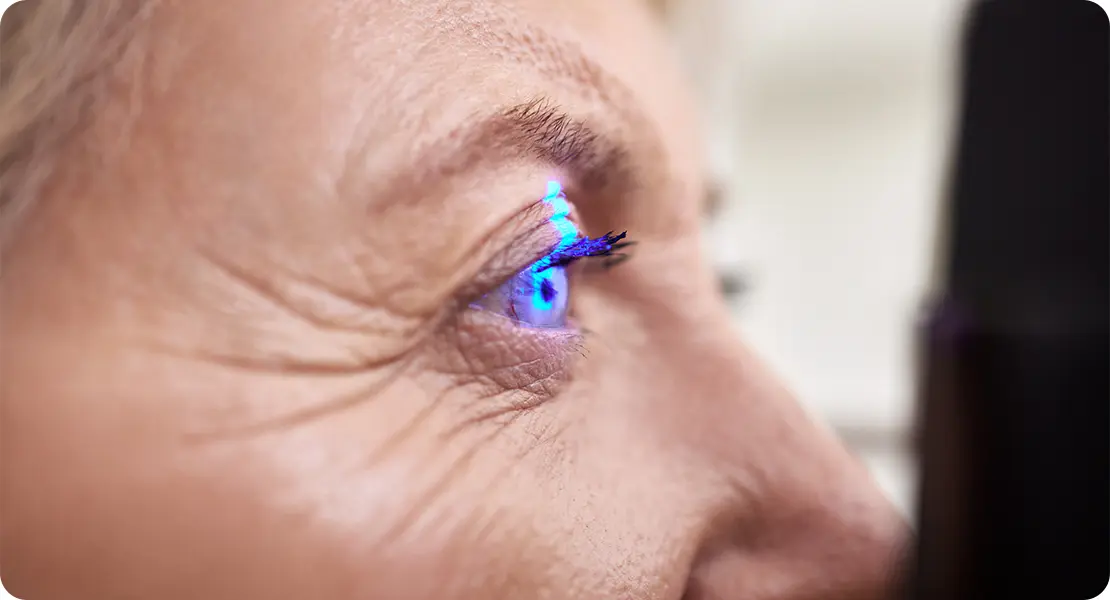
How your clinician will check things
Expect a dilated fundus examination with bright light and lenses to inspect your retina all the way to the periphery. If visibility is limited, an ocular ultrasound (B-scan) can help. Optical coherence tomography (OCT) may be used to check the macula for swelling or traction. If there’s any concern for a retinal tear, treatment is usually laser retinopexy or occasionally cryotherapy, performed urgently to prevent progression to detachment.
Management options for persistent, bothersome floaters
1) Watchful waiting
Many floaters settle below the central line of sight, move out of focus, or become less bothersome as the retinal image stabilises after surgery and your brain adapts. Because every intervention carries some risk, the default for mild to moderate symptoms is time, reassurance, and safety-net advice.
2) Treat the cause when one exists
If the examination finds a retinal tear, the priority is to seal it—usually with laser—to protect against detachment. If there’s vitreous haemorrhage, the strategy depends on the source and severity. If inflammation is present, anti-inflammatory drops may be adjusted.
3) YAG laser vitreolysis
This is a focused YAG laser used to disrupt certain floaters, most commonly a Weiss ring that sits well away from the retina and the lens implant. Outcomes vary, and some people still go on to need vitrectomy.
4) Pars plana vitrectomy
This surgical procedure removes the vitreous gel and the floaters within it. Modern techniques use small-gauge, sutureless approaches. When carefully selected, vitrectomy is the most definitive way to eliminate floaters, but it carries risks such as retinal detachment, bleeding, or infection.
Special situations
- High myopia: Retinas are thinner and risk of tears is higher, so vigilance is essential.
- Posterior capsular rupture: Floaters are more likely early on, and low thresholds for follow-up are sensible.
- After YAG capsulotomy: Tiny floaters are common; red-flag rules still apply.
- Multifocal or EDOF lenses: Can alter contrast perception, making floaters seem more noticeable.
- Diabetes or uveitis: Floaters may represent inflammatory cells or blood, so extra care is required.
Living with floaters: practical strategies
- Tame the background by using softer screen brightness or dark mode.
- Control glare with polarised sunglasses and peaked caps outdoors.
- Blink and lubricate with preservative-free artificial tears.
- Move the floater out of the way with small eye movements.
- Take regular breaks from screens to reduce fixation on artefacts.
Driving, work, and safety
A stable, mild floater is rarely a road-safety issue, but anything that suddenly obscures part of your field is different. Do not drive if you experience a sudden shower of floaters, flashes, or any shadow across your vision until you’ve been examined.
FAQs: Cataract Surgery and Persistent Floaters
1) Why did I only notice floaters after my cataract surgery?
Most people notice floaters more clearly after cataract surgery because the new lens implant allows sharper, brighter light to reach the retina. That makes shadows cast by the vitreous gel more obvious. In many cases, the floaters were present before surgery but hidden by the cloudy cataract lens.
2) How do I know if my floaters are harmless or a sign of something serious?
Harmless floaters usually appear as small specks or strands that drift in and out of view, especially against bright backgrounds. Serious symptoms include a sudden increase in floaters, flashing lights at the edge of vision, or a shadow or curtain coming across your sight. These can signal a retinal tear or detachment and need urgent assessment.
3) Can cataract surgery cause new floaters to develop?
Cataract surgery itself does not directly cause floaters, but changes in the vitreous gel sometimes occur afterwards. Some people develop a posterior vitreous detachment in the weeks or months following surgery, which can introduce new floaters. This is usually harmless, though it can occasionally lead to retinal tears that require treatment.
4) Are floaters after YAG capsulotomy different from those after cataract surgery?
Yes. After YAG laser treatment for posterior capsule opacification, it is common to see tiny flecks or dots drifting in your vision for a short time. These are usually fragments of capsule tissue that dissolve or drift out of sight. They tend to be temporary, but if you see a sudden increase in floaters or flashes, you should still get checked.
5) Do certain lens implants make floaters more noticeable?
Multifocal and extended depth of focus (EDOF) lenses can change the way light is distributed across the retina. Some patients find that floaters are more noticeable with these lenses compared to monofocals. This doesn’t mean the lens causes floaters; it is more about how your brain perceives contrast and detail through the implant.
6) Will floaters eventually go away on their own?
Floaters do not usually disappear completely, but they often become less intrusive. Over time, they can move out of your central vision, break up into smaller, less visible fragments, or your brain may simply learn to filter them out. For many people, floaters become far less noticeable within a few months of surgery.
7) What is YAG vitreolysis and when is it used?
YAG vitreolysis is a laser treatment that can break up or dissolve certain floaters, particularly a well-defined Weiss ring. It is only considered if the floater is dense, clearly visible, and safely positioned away from the retina and the lens implant. It is not suitable for people with multiple small or diffuse floaters.
8) What are the risks of vitrectomy for floaters?
Vitrectomy is a surgical procedure that removes the vitreous gel and all floaters with it. While very effective, it carries risks including retinal detachment, infection, and bleeding. Because of these risks, vitrectomy is generally only recommended for people whose floaters are severe, persistent, and significantly affecting their daily life.
9) Can floaters affect my ability to drive safely?
Mild, stable floaters are usually not a problem for driving, as your brain quickly adapts and filters them out. However, if you experience a sudden burst of floaters, flashing lights, or any shadow across your vision, you should not drive and should seek urgent eye assessment before getting back on the road.
10) When should I seek urgent medical help for floaters?
You should get urgent medical help if you suddenly see many more floaters than before, flashes of light, or a curtain-like shadow spreading across your vision. These can all be signs of a retinal tear or detachment, which need immediate treatment to protect your sight.
Final thoughts
Floaters after cataract surgery can be frustrating, especially when you were expecting nothing but clearer sight. The important thing is to know the difference between harmless specks that your brain will eventually learn to ignore, and the warning signs of something more serious like a retinal tear. Most of the time, patience and reassurance are all that’s needed, but treatments are available if floaters become a real barrier to daily life.
At London Cataract Centre, we see many patients with these concerns and always start with a thorough retinal check, clear advice on when to seek help, and a balanced discussion of treatment options. Whether you simply need reassurance, monitoring, or a more targeted approach, our team can guide you through the next steps with safety and comfort in mind.
References
- Hilford, D., Hilford, M., Mathew, A. & Polkinghorne, P.J. (2009) Posterior vitreous detachment following cataract surgery. Eye, 23(6), pp.1388–1392. Available at: https://www.nature.com/articles/eye2008273 (Accessed: 5 September 2025).
- Lin, T., Li, T., Zhang, X., Hui, Y., Moutari, S., Pazo, E.E., Dai, G. & Shen, L. (2021) The efficacy and safety of YAG laser vitreolysis for symptomatic vitreous floaters of complete PVD or non-PVD type. Ophthalmology and Therapy. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC8770727 (Accessed: 5 September 2025).
- Delaney, Y.M., Oyinloye, A. & Benjamin, L. (2002) Nd:YAG vitreolysis and pars plana vitrectomy: surgical treatment for vitreous floaters. Eye, 16(1), pp.21–26. Available at: https://www.nature.com/articles/6700026 (Accessed: 5 September 2025).
- Broadhead, G.K., Hong, T. & Chang, A.A. (2020) Management options for symptomatic vitreous floaters. Asia-Pacific Journal of Ophthalmology (Phila), 9(2), pp.96–103. Available at: https://www.sciencedirect.com/science/article/pii/S2162098923002153 (Accessed: 5 September 2025).
- The Royal Australian College of General Practitioners (2014) Flashes and floaters: a practical approach to assessment. Australian Family Physician. Available at: https://www.racgp.org.au/afp/2014/april/flashes-and-floaters (Accessed: 5 September 2025).