Cataract surgery is regarded as one of the safest and most transformative procedures in modern healthcare. In developed countries, it’s often completed in under 15 minutes and restores vision rapidly, sometimes even the same day. For many people, the idea of regaining clear sight feels almost routine. But this level of access isn’t universal, and millions still face preventable blindness simply because treatment is out of reach.
The economic divide plays a major role in this inequality. In high-income regions, insurance systems, government support and advanced surgical centres make cataract care widely available. Meanwhile, in low-income settings, the cost of surgery can equal several months’ wages, making it unaffordable for many families. Beyond cost, rural areas often lack clinics, equipment and trained surgeons, creating long waiting lists and overwhelming demand.
Even where the financial burden is reduced, logistical obstacles remain. Many patients live far from surgical centres, have limited transportation, or are unaware that cataracts are treatable. Cultural beliefs and fear of surgery can add further delays, allowing vision loss to progress until daily life becomes challenging. These barriers show that improving access is not just about lowering costs but also strengthening health systems and community education.
Thankfully, global initiatives are making a meaningful impact. Non-profit organisations are training local surgeons, building sustainable eye-care programmes and supplying low-cost lenses and equipment. Mobile eye camps and high-volume surgical models have dramatically improved efficiency in underserved regions. As technology becomes more affordable, the hope is that cataract surgery will eventually be accessible to everyone, regardless of geography or income.
Why Cataract Surgery Matters
Cataracts are the leading cause of blindness worldwide, affecting more than 100 million people. Without surgery, vision gradually worsens, impacting mobility, independence, and quality of life. Yet the procedure itself is simple and highly successful.
Modern cataract surgery takes just 15–30 minutes and restores vision in over 98% of cases. The problem isn’t the medicine it’s the ability to access it. For many people, especially in low-income regions, treatment remains out of reach.
While countries like the UK, US, and Japan offer routine cataract care through strong health systems, poorer regions struggle with cost, limited infrastructure, and too few trained surgeons. The biggest barrier isn’t technology it’s affordability and availability.
The Cost of Cataract Surgery Around the World

Cataract surgery costs vary dramatically across regions from under £25 in some low-cost programmes to over £3,000 in private hospitals. This disparity reflects differences in labour costs, surgical technology, healthcare funding models, and local economic structures.
In the United Kingdom, private cataract surgery typically costs between £1,800 and £3,000 per eye, although most cases are covered by the NHS. In the United States, the price is generally higher, ranging from around £2,500 to £4,000, depending on insurance coverage and hospital fees.
In contrast, cataract surgery in India is far more affordable, often costing between £20 and £250 per eye, particularly in charity-run or government-subsidised hospitals. Across Sub-Saharan Africa, the price can be as low as £10 in NGO-funded programmes but may rise to around £200 in private or semi-private clinics. Similarly, in Southeast Asia, the cost ranges from about £100 to £500, depending on whether the surgery is supported by public funding or charitable organisations.
These global differences reveal an important reality the cost of surgery alone doesn’t determine accessibility. Factors such as healthcare infrastructure, government subsidies, and the presence of outreach programmes play an equally vital role in ensuring patients receive sight-restoring care.
Public Health and Economic Barriers
Public health and economic barriers can significantly limit access to cataract surgery, even when the procedure itself is relatively affordable. Many patients struggle with long waiting lists, limited availability of specialised services, and shortages of trained surgeons in certain regions. On top of this, indirect costs such as travel, time off work, caregiver support, and follow-up appointments can make surgery harder to access for those on lower incomes. These challenges often delay treatment, worsen vision-related disability, and widen inequalities in eye care.
1. Lack of Trained Surgeons: In many developing countries, the ratio of ophthalmologists to population is as low as 1 per million. Rural regions may have no permanent eye specialist at all.
2. Limited Surgical Infrastructure: Operating theatres require reliable electricity, sterilisation, and precise instruments. Many community hospitals lack this infrastructure, especially outside major cities.
3. Awareness and Misconceptions: Cultural beliefs sometimes prevent people from seeking surgery. In some regions, cataract blindness is considered inevitable with age, rather than treatable.
4. Indirect Costs: Even when surgery is free, travel, accommodation, and lost work time can make treatment financially impossible for poor families.
5. Policy Gaps: Without strong national eye-care programmes, resources remain fragmented. Only 40% of low- and middle-income countries have integrated cataract care into public health plans.
Global Efforts to Improve Access
Global initiatives aimed at reducing cataract-related blindness have expanded rapidly over the past two decades, with governments, NGOs, and international health organisations working together to improve access. Many programmes focus on training local surgeons, increasing mobile surgical units, and subsidising treatment for low-income populations. Others work to strengthen supply chains, ensuring essential equipment and lenses are available even in remote regions. Together, these efforts are helping millions receive sight-restoring surgery who might otherwise have gone untreated.
1. The WHO’s Vision 2030 Initiative: The World Health Organization’s Vision 2030 aims to reduce avoidable blindness by strengthening national eye-care systems. Cataract surgery sits at the core of this strategy, with focus on training, infrastructure, and equitable financing.
2. The Aravind Model (India): The Aravind Eye Care System has revolutionised affordable eye surgery by standardising processes and scaling operations. Using an efficient, assembly-line model, it performs over 400,000 surgeries annually many for free or minimal cost while remaining financially self-sustaining.
3. Himalayan Cataract Project: Founded by Dr. Sanduk Ruit and Dr. Geoff Tabin, this project provides high-quality surgery in remote Himalayan regions using mobile surgical camps. They’ve restored vision for more than 1 million people using low-cost intraocular lenses (IOLs) manufactured locally.
4. Operation Eyesight Universal and Sightsavers: These NGOs build local capacity by training community health workers, funding cataract surgeries, and promoting awareness. Their outreach programmes in Africa and Asia continue to expand access in underserved areas.
The Role of Intraocular Lens (IOL) Innovation
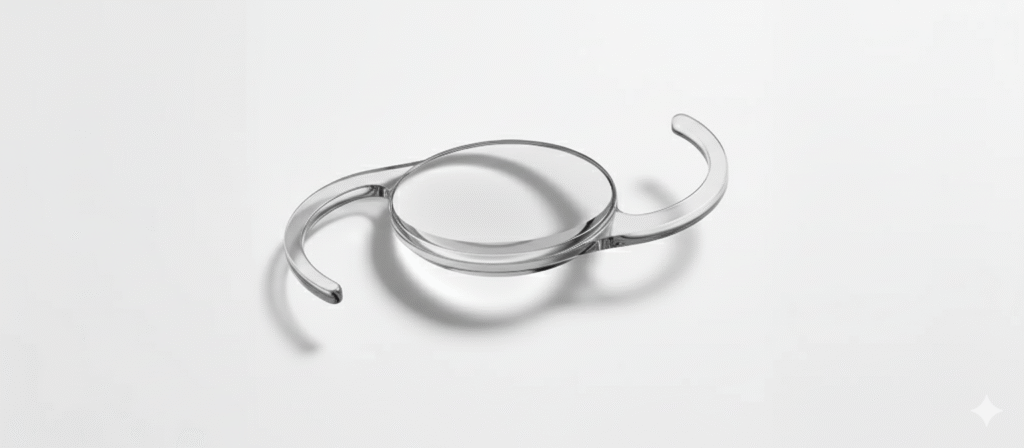
At the heart of cataract surgery is the intraocular lens a tiny artificial lens that replaces the eye’s cloudy natural one. Historically, IOLs were expensive to produce, driving up surgical costs. But technological advances and local manufacturing have drastically reduced prices.
Low-Cost IOL Production: Organisations like Aurolab in India now produce high-quality lenses for under £5, compared to £100–£300 for Western equivalents. These innovations allow large-scale surgeries at a fraction of the traditional cost.
Premium vs Standard Lenses: While developed countries often use multifocal or toric IOLs for advanced correction, affordable programmes typically focus on monofocal lenses simple, reliable, and effective for restoring functional vision.
Future Developments: Emerging research is exploring adjustable IOLs and 3D-printed lens technology, which could further cut manufacturing costs and personalise results in the next decade.
Mobile Cataract Surgery Units
Mobile cataract surgery units have transformed access to eye care by bringing fully equipped surgical facilities directly to underserved communities. They are designed to function just like a hospital operating theatre but on wheels.
These compact units include sterile environments, advanced microscopes, backup power, and all essential instruments required for safe cataract removal. This allows teams to deliver high-quality surgery even in remote locations.
The biggest advantage is cost reduction. Patients no longer need to travel long distances, take time off work, or arrange accommodation making treatment more affordable and accessible.
Countries such as India, Nepal, and Kenya have widely adopted these mobile units, helping restore sight to thousands who might otherwise remain blind due to lack of access.
The Economic Value of Cataract Surgery
Cataract surgery delivers far more than clearer vision it restores independence, mobility, and the ability to participate fully in daily life. By enabling people to see again, it reduces the burden on families and allows individuals to regain control over their routines.
Economically, the impact is remarkable. Research shows that every cataract operation can generate an average return of around 1,200%, thanks to improved productivity, fewer caregiving needs, and reduced long-term healthcare costs. This makes it a powerful investment for both communities and governments.
In developing regions, the benefits are even more visible. Adults can return to work, children no longer need to act as caregivers, and entire households regain financial stability. With such strong economic impact, the World Bank ranks cataract surgery among the most cost-effective health interventions worldwide.
How Developed Nations Manage Costs
In the UK, cataract surgery is widely accessible through the NHS, where it is fully or partially funded depending on clinical need. Private patients, however, may choose premium IOLs or faster appointments, with procedures ranging between £1,800 and £3,000 per eye.
Private facilities like London Cataract Centre offer advanced laser-assisted options, premium lenses, and precision outcomes within a transparent pricing structure ensuring both quality and accessibility in one of the world’s leading healthcare systems.
By contrast, patients in countries without public healthcare must rely on insurance or personal savings, making cataract treatment a financial burden for many.
Financing Models Improving Global Affordability
New financing approaches are helping more people access cataract care by reducing upfront costs and spreading expenses more sustainably. Micro-insurance schemes and community-based health funds now allow families to contribute small, regular payments that cover essential eye treatments when needed. Some regions use public–private partnerships to subsidise high-volume cataract centres, lowering surgical costs through economies of scale. In addition, outcome-based funding models where clinics receive support based on the number of successful surgeries are encouraging high-quality, high-efficiency care. Together, these innovative models are making cataract surgery more financially attainable for underserved populations.
1. Tiered Pricing Systems: Hospitals charge wealthier patients higher fees for premium lenses, which subsidise free or low-cost surgeries for those in need a model pioneered by Aravind and now replicated worldwide.
2. Microinsurance and Community Health Funds: Small-scale insurance schemes allow families to pool resources for affordable healthcare, including eye surgery. These have been successful in rural Kenya and Bangladesh.
3. Public-Private Partnerships (PPPs): Governments collaborate with NGOs and private clinics to deliver mass cataract campaigns. The Philippines and Vietnam have achieved major success with such hybrid models.
4. Local Manufacturing and Supply Chains: Producing IOLs, sutures, and viscoelastic materials locally reduces import costs and makes surgeries more self-sustaining for developing nations.
Technological Advances Lowering Costs
New technology is steadily lowering the overall cost of cataract surgery by making the process faster, more efficient and less resource-intensive. Automated phaco machines, improved imaging systems and AI-driven planning tools reduce time in theatre, increase accuracy and allow clinics to perform more surgeries safely each day. Portable surgical kits, smarter supply chains and remote follow-up systems also cut logistical expenses, helping deliver high-quality care at a fraction of the traditional cost.
1. Portable Phacoemulsification Systems
Modern portable phaco machines have transformed cataract care in remote and low-resource regions. These lightweight, battery-powered units allow surgeons to perform high-quality cataract surgery outside traditional hospital theatres, such as in outreach camps or rural clinics. Despite their compact design, they deliver the same level of safety and precision as standard hospital equipment, making eye care far more accessible.
2. AI and Teleophthalmology
Artificial intelligence and telemedicine now play a major role in early cataract detection. AI-driven tools can analyse retinal and lens images instantly, helping identify patients who need surgery long before symptoms become severe. Teleophthalmology reduces the need for long-distance travel, ensures better triage, and improves patient scheduling, particularly in areas with limited ophthalmologists.
3. Low-Cost Surgical Kits
Many centres have shifted from disposable surgical sets to reusable, sterilised kits. These durable toolkits significantly reduce surgical expenses while maintaining strict safety standards. In low-resource settings, this cost-effective approach allows for more surgeries to be performed, increasing access without compromising quality.
4. Laser-Assisted Systems
Although femtosecond laser platforms require a large initial investment, they offer exceptional accuracy in cataract surgery. These systems create precise incisions, soften the lens more efficiently, and improve overall surgical consistency. For high-volume clinics, laser-assisted cataract surgery enhances workflow, reduces variability, and delivers excellent long-term visual outcomes.
The Human Side of Affordability
Behind every cataract surgery lies a powerful human story of resilience and renewal. People who once struggled with even the simplest tasks suddenly regain clarity, confidence, and independence. It’s a reminder that vision isn’t just a sense it’s a lifeline.
Picture a grandmother in rural Nepal finally seeing her grandchildren’s faces clearly, or a Kenyan farmer returning to his fields after months of blindness. These stories are not rare; they mirror the experiences of millions whose lives have been transformed through affordable cataract care.
Cataract surgery is far more than a medical procedure it’s a restoration of dignity and opportunity. Each successful operation helps someone reclaim control over their life, rebuild connections, and step back into the world with renewed hope.
The Ethical Side of Global Access
Affordability isn’t just about cost it’s about fairness. The fact that a simple, curative surgery can mean the difference between sight and blindness raises ethical questions for the global medical community. Should modern medicine allow such disparities to exist? How can affluent health systems contribute to improving access elsewhere?
Many leading organisations now advocate for cross-subsidisation models and international collaboration, ensuring that profits from high-income care support lower-cost surgeries in underserved regions. It’s a small price for global equity in vision.
The Impact of COVID-19 on Access
COVID-19 had a profound impact on cataract care, causing widespread delays and cancellations across the world. In low-income regions, where services were already stretched thin, these disruptions pushed many patients into avoidable blindness.
To adapt, eye hospitals introduced digital triage, remote consultations, and staggered appointment systems. Mobile outreach camps also resumed with enhanced safety measures, helping reconnect patients with essential eye care.
As global recovery continues in 2026 and beyond, cataract surgery volumes are projected to exceed pre-pandemic numbers. Growing demand, new technologies, and strengthened outreach programmes are helping restore the momentum lost during the crisis.
Looking Ahead: The Future of Global Cataract Care
The future of global cataract care focuses on integration, automation, and wider access. Advances in technology and streamlined procedures are lowering costs and improving outcomes. Mobile units and telemedicine are expanding reach to underserved areas. Overall, the goal is high-quality, affordable care for everyone, everywhere.
AI-Assisted Diagnostics: Artificial intelligence can now identify cataracts from smartphone photos, helping remote screening teams prioritise patients faster.
Nanotechnology and Self-Adjusting Lenses: Experimental “light-adjustable lenses” could eliminate the need for glasses post-surgery, while maintaining affordability through mass production.
Universal Health Coverage (UHC): As more countries adopt UHC principles, cataract surgery is increasingly recognised as a basic healthcare right rather than a luxury procedure.
Sustainability Focus: Reusable surgical materials and eco-conscious supply chains are reducing the environmental footprint of large-scale cataract programmes.
FAQs:
1. Why is cataract surgery more expensive in some countries than others?
The cost of cataract surgery varies due to differences in healthcare systems, technology, labour costs, and government funding. In wealthier nations like the UK or the US, hospitals often use advanced laser-assisted systems, premium intraocular lenses, and highly trained specialists all of which increase the total cost. In contrast, developing countries such as India or Nepal often use simplified surgical techniques, locally produced lenses, and high-volume models to reduce expenses. Additionally, subsidies, charitable funding, and local manufacturing further lower costs, allowing many patients to receive surgery for a fraction of what it costs in Western nations.
2. Does a higher cost guarantee better results?
Not necessarily. While advanced equipment and premium lenses can enhance precision and visual outcomes, the surgeon’s skill and post-operative care are often more important than the price tag. In fact, some low-cost eye hospitals in India and Africa consistently achieve success rates comparable to those of private clinics in Europe. Affordable care models focus on efficiency and high surgical volumes without compromising on quality, demonstrating that good outcomes depend on expertise and process, not just expenditure.
3. What factors make cataract surgery inaccessible for millions of people worldwide?
The biggest barriers to cataract surgery are not purely financial. A shortage of trained ophthalmologists, limited hospital infrastructure, lack of awareness, and cultural misconceptions all contribute to inaccessibility. Many people in rural areas live hundreds of kilometres from the nearest surgical centre, and even when operations are free, the cost of travel, accommodation, and time away from work can be prohibitive. In some communities, misconceptions about surgery or fear of blindness also prevent people from seeking treatment, further deepening the access gap.
4. How are charities and NGOs helping to make cataract surgery more affordable?
Non-governmental organisations (NGOs) such as Sightsavers, Operation Eyesight Universal, and the Himalayan Cataract Project have transformed access by funding surgeries, training local teams, and setting up outreach camps in remote regions. These organisations often partner with local hospitals and governments to deliver free or low-cost procedures. By investing in sustainable programmes and community education, they not only provide immediate care but also create long-term systems that continue functioning independently after external funding ends.
5. What role does technology play in lowering cataract surgery costs?
Technological innovation has been a major driver in making cataract surgery more affordable and accessible. Portable phacoemulsification machines allow high-quality surgeries to be performed even outside urban hospitals. Locally manufactured intraocular lenses, costing less than £5, have replaced expensive imports. AI-assisted diagnostic tools are now helping identify cataract cases earlier, while teleophthalmology enables remote consultations, saving patients unnecessary travel. Together, these advances reduce both direct and indirect costs, making surgery feasible for millions more people.
6. How do mobile cataract surgery units work, and are they safe?
Mobile surgical units are fully equipped, sterile environments designed to bring cataract surgery directly to patients in rural or underserved areas. These units include microscopes, power backups, and sterilisation facilities, ensuring hospital-level safety and precision. Surgeons travel with their teams to remote communities, performing same-day operations before moving to the next location. The approach has been widely successful in countries such as Nepal and Kenya, where mobile units have restored sight to thousands who otherwise would have had no access to surgery. Safety standards are strictly maintained, often matching those of permanent eye hospitals.
7. What makes the Aravind Eye Care System a global model for affordability?
The Aravind Eye Care System in India has become a global benchmark for cost-effective cataract care through its innovative tiered pricing and high-volume efficiency. Patients who can afford to pay choose private rooms and premium lenses, while the revenue from these services subsidises free surgeries for low-income individuals. By standardising every step of the process from lens manufacturing through its partner company Aurolab to streamlined surgical protocols Aravind has achieved world-class outcomes at minimal cost. Its model has been studied and replicated in multiple countries, demonstrating that compassion and efficiency can coexist in modern medicine.
8. How does cataract surgery contribute to the economy in developing countries?
Restoring sight has profound economic benefits. A successful cataract operation allows adults to return to work, increases household income, and frees children from caregiving responsibilities, allowing them to return to school. Studies estimate that for every £1 invested in cataract surgery, there is a return of roughly £12 in economic productivity and social value. On a broader scale, national productivity improves as fewer people depend on social or family support, and communities become more self-sufficient. Thus, cataract surgery is not only a medical intervention but also a catalyst for economic growth.
9. Can cataract surgery completely eliminate blindness worldwide?
In theory, yes because cataract blindness is entirely preventable and curable with timely surgery. The challenge lies in equitable access, especially in low-resource settings. With adequate funding, training, and infrastructure, global blindness caused by cataracts could be virtually eradicated. WHO’s Vision 2030 initiative aims precisely at this goal, advocating for universal access to essential eye care and integrating cataract surgery into national healthcare systems. Success stories in countries like India and Nepal prove that large-scale elimination of cataract blindness is achievable when resources are strategically directed.
10. What is the future of global cataract care and affordability?
The future of cataract surgery is being shaped by a combination of innovation, inclusivity, and sustainability. Artificial intelligence and smartphone-based screening are making diagnosis easier in remote regions. Advances in nanotechnology are leading to the development of self-adjusting lenses, which could reduce the need for glasses after surgery. Governments are increasingly including cataract care under universal health coverage, recognising it as a basic human right. At the same time, the focus is shifting toward eco-friendly surgical practices, such as reusing instruments safely to reduce waste. These trends suggest that over the next decade, cataract surgery will become more accessible, affordable, and environmentally conscious than ever before.
Final Thoughts: Restoring Sight, Strengthening Futures
Cataract surgery is more than a medical breakthrough it’s a social and economic equaliser. Around the world, it continues to prove that affordable healthcare can transform entire communities, not just individuals. From large-scale outreach programmes in Asia and Africa to technological innovation and public-private partnerships, progress is being made toward a future where no one loses vision because of cost or access barriers.
If you’re considering cataract surgery in London, you can get in touch with us at London Cataract Centre. Our expert ophthalmologists provide world-class care using the latest techniques and technology, helping you regain clear vision with confidence.
References:
1. Lansingh, V.C., Carter, M.J. & Martens, M. (2007). Global cost-effectiveness of cataract surgery. Ophthalmology, 114(9), pp.612–620. Available at: https://pubmed.ncbi.nlm.nih.gov/17306903/
2. Flessa, S., Heiduschka, P., Hecht, L. & Korn, D. (2022). Cataract surgery in low-income countries: a good deal! Healthcare, 10(12), p.2580. Available at: https://www.mdpi.com/2227-9032/10/12/2580
3. Aravind, S. (2008). Cataract surgery and intraocular lens manufacturing in India. Indian Journal of Ophthalmology, 56(4), pp.335–341. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2636088/
4. Fang, J., Wang, X., Lin, Z. et al. (2010). Variation of cataract surgery costs in four different graded providers of China. BMC Public Health, 10, Article 543. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2949733/ 5. Wang, W., Zhang, Y. & Zheng, Y. (2016). Cataract surgical rate and socio-economics: a global study. Investigative Ophthalmology & Visual Science, 57(14), pp.5720–5728. Available at: https://pubmed.ncbi.nlm.nih.gov/27802536/

