If you have glaucoma and have been told you need cataract surgery, it is very normal to feel worried about risk. Many patients assume that having glaucoma automatically makes cataract surgery dangerous or unpredictable. When your sight already feels fragile, the idea of surgery can understandably feel unsettling.
The reality is more reassuring than many people expect. Cataract surgery in glaucoma patients is common and, when planned carefully, is usually safe and effective. The key difference is not whether surgery should be done, but how it is approached.
In this article, we explain honestly whether cataract surgery is riskier when you have glaucoma, which risks are genuinely higher, how surgeons adapt techniques for glaucoma eyes, and why careful planning usually leads to stable, predictable outcomes. Our aim is to replace fear with clarity so you can move forward with confidence.
Understanding the Relationship Between Glaucoma and Cataracts
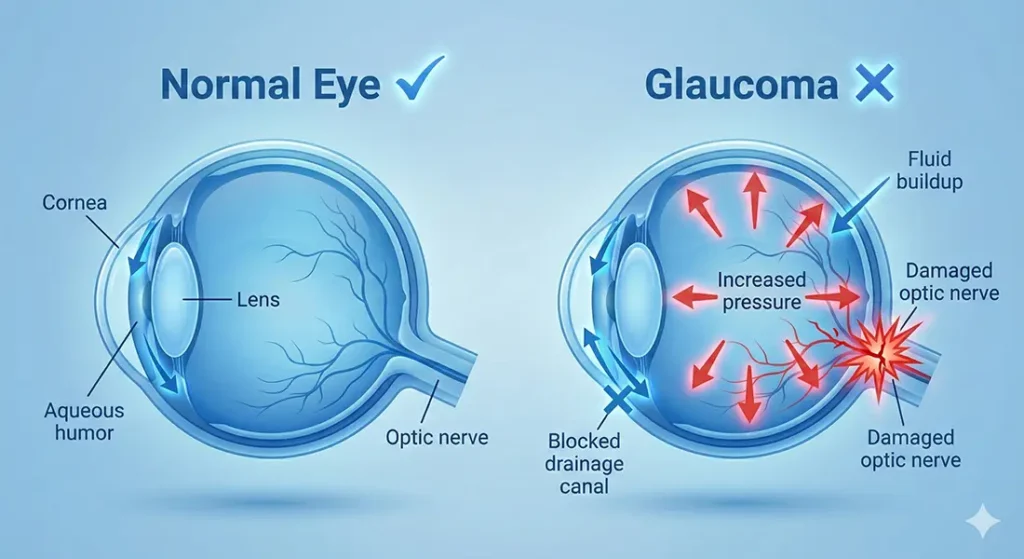
Glaucoma and cataracts often occur together, especially as we get older. Glaucoma affects the optic nerve, while cataracts affect the clarity of the natural lens. Although they involve different parts of the eye, they influence each other clinically.
Many glaucoma patients eventually develop cataracts either as part of natural ageing or as a side effect of long-term eye drop use. This means surgeons regularly treat patients who have both conditions.
Because this combination is so common, modern cataract surgery techniques are well adapted to managing glaucoma safely.
Why Glaucoma Makes Patients More Anxious About Surgery
Glaucoma understandably changes how you feel about eye surgery. Because vision loss can happen slowly and irreversibly, anything involving the eye can feel risky. This anxiety is common, valid, and something we take seriously during surgical planning.
Here’s why concerns tend to be higher in glaucoma:
1. Glaucoma Is Often a “Silent” Condition – Vision loss can progress gradually without obvious symptoms. This uncertainty makes many patients feel protective of their eyes and cautious about any intervention.
2. Fear of Optic Nerve Damage – Many patients worry that surgery could worsen glaucoma or harm the optic nerve. Because the optic nerve cannot recover once damaged, this fear carries real emotional weight.
3. Concerns About Pressure Spikes – Some people are anxious that surgery might cause sudden rises in eye pressure. Others worry that complications would have more serious consequences than in a healthy eye.
4. Higher Stakes Feel More Personal – When you already live with an eye condition, the idea of “something going wrong” can feel more threatening. Even low-risk procedures may feel emotionally heavier.
These concerns are valid, but they need context. When we understand how glaucoma eyes are assessed, protected, and monitored, real risks become clearer and assumptions fall away. Careful planning allows us to minimise risk and move forward with confidence rather than fear.
Top of Form
Bottom of Form
Is Cataract Surgery Inherently Riskier in Glaucoma?

Cataract surgery is not automatically high-risk just because you have glaucoma. For many patients, the overall safety profile remains very good, and outcomes are often comparable to those without glaucoma. We don’t assume increased risk without looking at the full picture.
That said, certain aspects do need extra attention. We carefully consider how eye pressure behaves during and after surgery, how resilient the optic nerve is, and how your eye responds to inflammation. These factors guide how we plan and monitor your care.
When these considerations are recognised early and managed proactively, surgery is usually very safe. We focus on anticipating challenges rather than reacting to them. This structured approach helps protect your vision and supports a smooth recovery.
Which Risks Are Genuinely Higher in Glaucoma Patients
Some risks are slightly increased in glaucoma patients, and it is important to be honest about them. Temporary changes in eye pressure after surgery are more common and need closer monitoring.
There may also be a higher sensitivity to inflammation, especially in eyes that have been treated with long-term drops or previous glaucoma surgery. In advanced glaucoma, the optic nerve has less reserve, meaning sudden pressure changes matter more.
These risks are well understood and routinely managed. Awareness, not avoidance, is what keeps surgery safe.
Eye Pressure Changes After Cataract Surgery
One of the most discussed concerns is eye pressure after cataract surgery. In the short term, pressure can rise or fall as the eye heals. In glaucoma patients, surgeons monitor this closely because pressure spikes can stress the optic nerve. Modern surgical techniques and medications are specifically designed to minimise these fluctuations. Interestingly, cataract surgery can also lower eye pressure in some glaucoma patients over the long term, which can be a positive secondary benefit.
How Surgeons Adapt Techniques for Glaucoma Eyes
Cataract surgery is never a one-size-fits-all procedure, especially when glaucoma is present. Surgeons adjust their technique to account for the eye’s increased sensitivity and the need for pressure stability. These refinements are part of established glaucoma-aware care, not experimental steps.
Surgical techniques are adapted in glaucoma because:
- Fluid settings are adjusted carefully – Gentler fluid dynamics help avoid sudden pressure changes during surgery.
- Surgical time is managed deliberately – Efficient, controlled procedures reduce stress on the eye and optic nerve.
- Techniques minimise intraocular stress – Every step is designed to protect delicate structures while maintaining stability.
- Adjustments follow established practice – These methods are standard in glaucoma-focused cataract care, not experimental or unproven.
By tailoring surgical technique to the needs of glaucoma eyes, surgeons prioritise safety, pressure control, and long-term visual health.
The Importance of Pre-Operative Assessment
When glaucoma is present, careful pre-operative assessment becomes even more important. This stage is where we identify potential risks, understand how your eyes function, and plan surgery in a way that protects your remaining vision. Good assessment is the foundation of safe decision-making.
Here’s why this step matters so much:
1. Glaucoma Severity Must Be Clearly Understood – We assess how advanced the glaucoma is and whether it is stable. Early, well-controlled glaucoma carries very different considerations compared to more advanced disease.
2. Visual Fields and Optic Nerve Health Are Reviewed – Looking at visual field tests and optic nerve scans helps us understand how much functional vision is present. This information guides how cautiously we approach surgery.
3. Stability Is Just as Important as Diagnosis – A stable condition allows for more predictable outcomes. If glaucoma is fluctuating or progressing, we may adjust timing or surgical strategy accordingly.
4. Surgery Is Planned for Your Eye, Not an Average One – Pre-operative assessment ensures decisions are tailored to your specific eye health. We don’t rely on general rules or assumptions when glaucoma is involved.
This detailed assessment allows us to balance benefit and risk thoughtfully. By understanding your glaucoma in depth, we can plan surgery that respects the health of your optic nerve and supports the best possible visual outcome.
Why Glaucoma Severity Matters More Than the Diagnosis Itself
Glaucoma is not a single, uniform condition. Early, well-controlled glaucoma behaves very differently from advanced disease with significant visual field loss. We always look at where you sit on that spectrum rather than focusing on the label alone.
In early glaucoma, the optic nerve usually tolerates cataract surgery very well. In more advanced glaucoma, the nerve is more vulnerable, so we take additional precautions before, during, and after surgery. This careful approach helps reduce stress on the eye.
Risk is therefore linked more to severity and stability than to the simple presence of glaucoma. We base decisions on how the disease is behaving now and how robust the optic nerve is. This personalised assessment allows us to plan surgery more safely and confidently.
Visual Field Loss and Surgical Planning
Visual field loss means parts of your vision are already missing. Cataract surgery does not restore these areas, but it can improve clarity in the remaining field. Surgeons plan surgery carefully to avoid any unnecessary stress that could affect remaining vision. This includes managing pressure carefully and avoiding prolonged surgical time. The goal is to preserve and optimise the vision you have, not to chase unrealistic improvements.
Contrast Sensitivity and Visual Expectations
Glaucoma can affect how crisp and clear your vision feels, even when standard eyesight tests seem reasonable. This is often due to reduced contrast sensitivity rather than sharpness alone. Understanding how cataract surgery influences contrast helps set realistic and reassuring expectations.
Here’s how contrast sensitivity fits into the picture:
1. Glaucoma Can Reduce Contrast Sensitivity – Glaucoma affects the optic nerve, which can make it harder to distinguish subtle differences between light and dark. This is why vision may feel “washed out” or less sharp, even before cataracts become severe.
2. Cataracts Further Reduce Contrast – A cloudy lens scatters light and reduces contrast even more. This often compounds the visual difficulties already caused by glaucoma.
3. Cataract Surgery Often Improves Contrast – By removing the cloudy lens, cataract surgery usually allows more light to pass cleanly into the eye. In most cases, this improves contrast rather than making it worse.
4. Expectations Need to Be Balanced – While surgery cannot reverse optic nerve damage, it can optimise the clarity of the image reaching the nerve. Understanding this helps align expectations with what surgery can realistically achieve.
When patients understand how contrast works, anxiety often reduces. Cataract surgery is about improving the quality of the image entering the eye, not increasing risk. With clear explanations and realistic goals, we can approach surgery with confidence rather than fear.
Combined Cataract and Glaucoma Surgery
In some situations, cataract surgery may be combined with a glaucoma procedure. We usually consider this when eye pressure control needs improvement alongside cataract removal. Combining procedures can be a thoughtful, planned decision rather than a routine step.
Combined surgery does slightly change the risk profile, and we take this into account carefully. At the same time, it can offer clear advantages, such as better pressure control and a reduced reliance on glaucoma medications. We assess whether the benefits outweigh the added complexity for you as an individual.
When done for the right reasons, combined surgery can be both safe and effective. We focus on stability, long-term eye health, and reducing treatment burden where possible. Clear explanation helps you feel confident about why this approach may be recommended.
Inflammation and Healing in Glaucoma Eyes
Eyes affected by glaucoma can be more sensitive to inflammation, especially if pressure-lowering drops have been used for many years. We take this into account when planning surgery and recovery. The aim is to minimise stress on already sensitive tissues.
Post-operative anti-inflammatory drops are often tailored rather than routine. We adjust treatment to support calm healing and reduce the risk of pressure fluctuation or prolonged irritation. Close follow-up allows us to respond quickly if the eye reacts unexpectedly.
With appropriate planning and monitoring, healing is usually smooth and predictable. We focus on preventing problems rather than reacting to them. This careful approach helps protect the optic nerve and supports a comfortable recovery.
Medication Considerations Before and After Surgery
Glaucoma medications remain an important part of care before and after cataract surgery. Managing these drops carefully helps keep eye pressure stable while your eye heals. This process is routine and carefully planned, not something left to chance.
Here’s how medication is usually managed:
1. Some Glaucoma Drops Are Continued – Many pressure-lowering drops are continued straight through the surgical period. These help maintain stable eye pressure and protect the optic nerve.
2. Others May Be Adjusted Temporarily – Certain medications may be paused or adjusted around the time of surgery. This is done to support healing and avoid unnecessary irritation or interaction with post-operative drops.
3. Clear Communication Keeps Pressure Stable – We make sure you know exactly which drops to use and when. Clear instructions reduce confusion and help maintain consistent pressure control.
4. Close Monitoring Follows Surgery – After surgery, pressure is checked regularly to ensure medications are working as expected. If adjustments are needed, they are made early and carefully.
Medication management is a standard part of glaucoma-aware cataract care. By monitoring pressure closely and tailoring treatment to your eye’s response, we protect healing and long-term vision. This careful approach allows surgery to proceed safely while keeping your glaucoma well controlled.
Does Cataract Surgery Worsen Glaucoma?
Eyes affected by glaucoma can be more sensitive to inflammation, especially if pressure-lowering drops have been used for many years. We take this into account when planning surgery and recovery. The aim is to minimise stress on already sensitive tissues.
Post-operative anti-inflammatory drops are often tailored rather than routine. We adjust treatment to support calm healing and reduce the risk of pressure fluctuation or prolonged irritation. Close follow-up allows us to respond quickly if the eye reacts unexpectedly.
With appropriate planning and monitoring, healing is usually smooth and predictable. We focus on preventing problems rather than reacting to them. This careful approach helps protect the optic nerve and supports a comfortable recovery.
The Role of Surgeon Experience
Experience plays a crucial role when operating on eyes affected by glaucoma. Surgeons who regularly manage glaucoma understand how to adapt surgical technique, pacing, and aftercare to protect the optic nerve. This familiarity allows decisions to be made calmly and confidently.
We see that experience reduces risk and improves predictability. Subtle adjustments during surgery and tailored post-operative care can make a meaningful difference to outcomes. These details are often invisible to patients but are essential for safety.
Choosing a clinic that routinely treats glaucoma patients provides added reassurance. Skill and planning work together to keep outcomes safe and recovery smooth. This depth of experience helps protect vision both now and in the future.
What Patients Often Misunderstand About Risk
It’s common to think that higher risk automatically means surgery should be avoided. In reality, avoiding treatment can sometimes create different risks that are just as important. When cataracts progress, they can affect both daily quality of life and how well we monitor glaucoma.
Risk is often misunderstood because:
- Untreated cataracts affect more than vision – Reduced lens clarity can make everyday tasks harder and increase visual strain.
- Glaucoma monitoring becomes less reliable – Poor clarity can interfere with accurate pressure checks and optic nerve assessment.
- Surgery can support glaucoma management – In some cases, cataract surgery actually improves examination quality and pressure control.
- Risk is about balance, not avoidance – Decisions are made by weighing the risks of surgery against the risks of doing nothing.
By understanding this balance, you can see cataract surgery as part of comprehensive eye care rather than a threat, helping you make more confident, informed decisions.
How Follow-Up Care Protects Vision
Post-operative follow-up is especially important when glaucoma is present. We schedule regular pressure checks and visual assessments to make sure your eye is responding as expected. This careful monitoring protects the optic nerve during recovery.
This follow-up period is proactive rather than reactive. We aim to identify small changes early, before they develop into larger problems. Early adjustment keeps healing on track and reduces risk.
Close follow-up is one of the main reasons outcomes are usually stable and predictable. We focus on continuity of care, not just the surgery itself. Ongoing review helps protect your vision in both the short and long term.
Asking the Right Questions Before Surgery
Before surgery, it’s helpful to ask how your stage of glaucoma affects risk and what specific precautions will be taken. We encourage these conversations because understanding the plan builds confidence and trust. Clarity helps you feel more in control.
It’s also important to ask how eye pressure will be monitored after surgery and which symptoms should prompt urgent review. Knowing what to expect reduces uncertainty and anxiety during recovery. We believe informed patients recover more comfortably.
When questions are addressed openly, the entire process feels more secure. We value clear communication at every stage of care. Feeling informed helps you move through surgery and recovery with greater reassurance.
The Role of Specialist Centres
Cataract surgery in patients with glaucoma benefits greatly from specialist oversight. We know that clinics experienced in managing both conditions can coordinate care more safely and effectively. This integrated approach reduces uncertainty and improves confidence.
At London Cataract Centre, cataract surgery for patients with glaucoma is planned with careful assessment, pressure-aware surgical techniques, and structured follow-up. We consider optic nerve health, pressure behaviour, and long-term stability at every step.
This specialist-led approach helps you feel reassured rather than at risk. By combining expertise, planning, and close monitoring, we support safe, predictable outcomes and protect the vision you rely on every day.
Balancing Risk Against Quality of Life
Risk should always be considered in context, not in isolation. Living with significant cataract symptoms can affect your independence, confidence, and overall wellbeing just as much as any medical risk. The aim is to weigh what you gain against what you accept.
Balancing risk and quality of life matters because:
- Untreated symptoms affect daily independence – Difficulty with reading, driving, or recognising faces can quietly limit your lifestyle.
- Surgery can offer meaningful improvement – When cataracts interfere with everyday life, treatment can restore function and confidence.
- Glaucoma requires thoughtful planning, not avoidance – With careful assessment and technique, benefits can often be achieved safely.
- The goal is intelligent risk management – We don’t aim to eliminate all risk, but to understand and manage it responsibly.
By weighing benefit against risk in a structured way, we help you make decisions that support both safety and quality of life.
FAQs
1. Is cataract surgery genuinely more dangerous if I have glaucoma?
Cataract surgery is not automatically dangerous just because you have glaucoma. For most patients, it remains a safe and commonly performed procedure. The key difference is that surgery is planned more carefully to protect eye pressure and the optic nerve.
2. What is the main additional risk glaucoma patients face during cataract surgery?
The most important additional consideration is eye pressure fluctuation around the time of surgery. Glaucoma eyes are more sensitive to sudden pressure changes, which is why surgeons monitor and manage pressure very closely before and after the procedure.
3. Can cataract surgery make my glaucoma worse?
Cataract surgery does not usually worsen glaucoma when planned properly. In fact, many patients experience stable glaucoma control after surgery, and some even see a small long-term reduction in eye pressure. Careful monitoring ensures any changes are addressed early.
4. Why does glaucoma severity matter more than just the diagnosis itself?
Early, well-controlled glaucoma behaves very differently from advanced disease. In advanced glaucoma, the optic nerve has less tolerance for stress, so surgeons take extra precautions. Risk is therefore linked to severity and stability, not simply having the condition.
5. Will cataract surgery still improve my vision if I already have glaucoma damage?
Cataract surgery cannot reverse optic nerve damage, but it often improves the clarity and brightness of the vision you still have. Removing the cloudy lens allows a cleaner image to reach the optic nerve, which many patients find significantly improves daily function.
6. Are pressure spikes after surgery common in glaucoma patients?
Temporary pressure changes can occur after cataract surgery, and they are slightly more common in glaucoma patients. These changes are usually short-lived and closely monitored. Modern techniques and medications are designed specifically to keep pressure stable.
7. Does cataract surgery ever help with glaucoma control?
In some patients, cataract surgery leads to a modest long-term reduction in eye pressure. While it is not a treatment for glaucoma itself, this pressure-lowering effect can be a helpful secondary benefit in certain cases.
8. Is combined cataract and glaucoma surgery riskier than cataract surgery alone?
Combined surgery does involve more complexity, but it is often chosen deliberately for the right patients. When pressure control is needed, combining procedures can reduce medication burden and improve stability. Careful planning keeps outcomes predictable and safe.
9. Does recovery take longer if you have glaucoma?
Recovery is often similar to that of patients without glaucoma, but follow-up is more intensive. Pressure checks and medication adjustments are done more frequently to protect the optic nerve. This closer monitoring improves safety rather than slowing recovery.
10. How can I reduce my risk before and after cataract surgery?
Attending all pre-operative assessments, following medication instructions carefully, and keeping follow-up appointments are essential. Open communication about symptoms and concerns also helps surgeons respond quickly if adjustments are needed. Good planning and cooperation significantly reduce risk.
Final Thoughts: Clear Risk, Careful Planning, Safer Outcomes
Cataract surgery in people with glaucoma is rarely about avoiding treatment and far more about planning it properly. When glaucoma severity, optic nerve health, and eye pressure behaviour are carefully assessed, surgery is usually safe, predictable, and beneficial. Understanding how risk is managed helps replace fear with confidence and allows decisions to be made based on clarity rather than assumption. If you’re thinking about Glaucoma treatment in London, you can get in touch with us at London Cataract Centre.
References
1. Premium intraocular lenses in glaucoma a systematic review, Bioengineering, 10(9), 993. https://www.mdpi.com/2306-5354/10/9/993
2. Central contrast sensitivity as an outcome measure in randomized controlled trials in glaucoma a systematic review, Life, 15(7), 1043. https://www.mdpi.com/2075-1729/15/7/1043
3. Kitnarong, N., Udomwech, L., Chongthurakit, N., Phongsuphan, T. & Petchyim, S. (2023) Effects of blue-light-filtering intraocular lenses on contrast sensitivity in patients with glaucoma, Medicine (Baltimore), e36821. https://pmc.ncbi.nlm.nih.gov/articles/PMC10754553/
4. Premium Intraocular Lenses in Glaucoma A Systematic Review (PubMed abstract). https://pubmed.ncbi.nlm.nih.gov/37760095/
5. Multifocal, toric, and aspheric intraocular lenses for glaucoma patients (abstract). https://pubmed.ncbi.nlm.nih.gov/21507514/

