If you’ve had cataract surgery, you might have been told about something called a “secondary cataract.” The proper term for it is posterior capsule opacification (PCO), and it happens when the thin capsule that holds your artificial lens becomes cloudy over time. This cloudiness can cause blurred vision, glare, or even a return of the same symptoms that pushed you to have cataract surgery in the first place.
The good news is that there’s a straightforward outpatient procedure to treat it: YAG laser capsulotomy. It only takes a few minutes, involves no cutting or stitches, and clears up the haze almost immediately. But the big question many people ask is this: what’s the success rate? In other words, how likely is it to work, how long will it last, and are there risks you should know about?
In this article, we’ll break down the success rate of YAG laser capsulotomy in detail. We’ll explore the evidence, talk about what success really means in practical terms, look at factors that influence outcomes, and answer common questions patients have. By the end, you’ll have a clear picture of what to expect if you’re considering or preparing for this laser treatment.
Understanding YAG Laser Capsulotomy
Before diving into statistics, it’s worth understanding exactly what this procedure does.
During cataract surgery, your cloudy natural lens is removed but the capsule (a thin membrane around the lens) is left behind. The new artificial intraocular lens (IOL) is placed inside this capsule. Over time, residual lens cells can migrate across the capsule, leading to clouding or wrinkling. That’s what we call posterior capsule opacification.
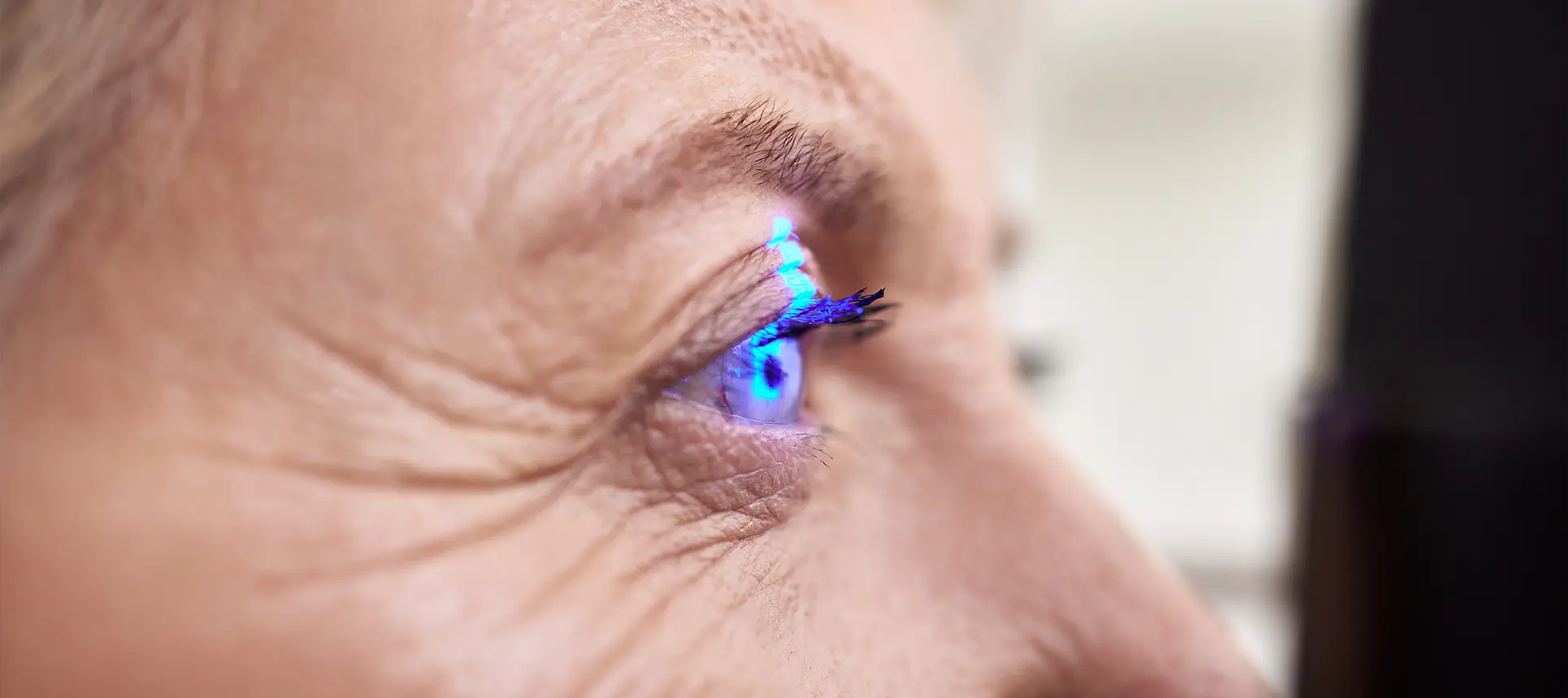
When this happens, vision that was once crisp after surgery can gradually blur again. YAG laser capsulotomy fixes this by creating a small, central opening in the back of the capsule using pulses of laser light. The opening allows light to pass freely to the retina again, restoring clarity.
The procedure is painless (anaesthetic drops are used), quick, and done in the clinic. There are no stitches, and most people notice an improvement within 24 to 48 hours.
Reported Success Rates

When we talk about the “success rate,” we’re usually looking at two things:
- Immediate improvement – how many patients notice clearer vision straight after the procedure.
- Long-term outcomes – how many keep that clarity without complications or further treatment.
Immediate success
Studies consistently report that over 95% of patients experience meaningful visual improvement after YAG capsulotomy. For most, it’s almost like lifting a fog. Colours look brighter, reading becomes easier, and glare is reduced.
Long-term outcomes
The benefit is usually long-lasting. Once the opening is made in the capsule, it rarely clouds over again. Recurrence is very uncommon, though in a small number of cases extra treatment may be needed if haze forms at the edges of the opening.
Large-scale studies show that most patients retain their improved vision for years. A minority may develop floaters, mild inflammation, or in very rare cases, complications such as retinal detachment. But these risks remain low.
What “Success” Actually Means
Success isn’t the same for everyone. Here are the main aspects to consider:
- Clarity of vision: For most, YAG restores sight back to the level it was after cataract surgery.
- Speed of improvement: Vision often sharpens within a day or two, making it one of the fastest ways to regain clarity.
- Durability: Once treated, most people don’t need the procedure again.
- Safety: The complication rate is low, which contributes to its high success rate overall.
If you have other eye conditions such as glaucoma, macular degeneration, or diabetic retinopathy, the improvement may not be as dramatic. YAG clears the capsule, but it cannot fix unrelated eye problems.
Factors That Influence the Success Rate
Not every patient’s outcome will be identical. Here are some of the key factors:
Lens type
The kind of intraocular lens used during your cataract surgery plays a big role. Modern hydrophobic acrylic lenses with sharp edges are less likely to allow cell migration, so patients with these lenses often have a lower chance of PCO and therefore need fewer YAG procedures.
Surgical technique
How well the original cataract surgery was performed also matters. If the lens capsule was cleaned thoroughly and the IOL positioned correctly, there’s less chance of the capsule becoming cloudy.
Patient factors
Younger patients, or those with inflammatory eye conditions, may develop PCO sooner and sometimes more aggressively. Diabetics are also at slightly higher risk.
Surgeon’s skill with the laser
An experienced ophthalmologist will create a clean, central, well-sized opening, which reduces the risk of glare, floaters, or the need for repeat procedures.
Risks and Complications
Although YAG capsulotomy has a very high success rate, it’s not entirely without risk. Possible issues include:
- Floaters: Tiny specks may appear in your vision after the procedure. These usually settle down within weeks.
- Pressure spikes: Eye pressure can rise temporarily, which is why it’s sometimes checked after the laser.
- Inflammation: Mild inflammation can occur but usually responds quickly to drops.
- IOL damage: Rarely, the laser can mark the artificial lens, but this usually doesn’t affect vision.
- Retinal detachment: Very rare but the most serious risk. Patients with high myopia (very long-sighted eyes) are slightly more at risk.
Even with these risks, the vast majority of patients come through the procedure without any significant problems.
What to Expect During and After

The procedure itself is straightforward. You’ll sit at a laser machine similar to the one used for eye checks. After anaesthetic drops, the surgeon applies laser pulses to create the capsule opening. It usually takes less than five minutes.
Afterwards, you may notice floaters or slight blurriness from the drops, but many people see better almost immediately. Normal activities can usually be resumed the next day. Follow-up appointments are used to check eye pressure and healing.
Frequently Asked Questions
1. How effective is YAG laser capsulotomy?
YAG laser capsulotomy is one of the most reliable eye procedures available, with success rates typically reported above 95%. In practical terms, that means nearly all patients see a noticeable improvement in clarity and reduction of glare soon after the treatment. The laser works by creating a permanent opening in the capsule that allows light to reach the retina without obstruction. While success can vary depending on other eye conditions such as macular degeneration or glaucoma, the vast majority of people achieve vision that returns close to the sharpness they enjoyed immediately after cataract surgery.
2. Will I ever need the treatment again?
For most people, a single YAG laser capsulotomy is enough to keep vision clear for life. Once the cloudy capsule has been opened, it does not usually regrow or become opaque in the same spot. In rare situations, however, haze can form around the edges of the laser opening, or the initial opening may have been too small, meaning a second procedure is required. These repeat cases are uncommon, but it is reassuring to know that if further treatment is needed, the same laser procedure can be performed again safely and effectively.
3. How quickly will I notice improvement?
One of the most remarkable aspects of YAG capsulotomy is the speed of recovery. Many people walk out of the clinic noticing that their vision is already clearer, while others find that the full improvement becomes obvious after a day or two, once the pupil returns to normal from the dilating drops and any temporary floaters settle down. For activities such as reading, driving, or using digital devices, the difference can feel dramatic almost overnight, making it one of the fastest ways to restore lost clarity of sight.
4. Is YAG laser capsulotomy painful?
The procedure itself is not painful. Your ophthalmologist will apply anaesthetic drops to completely numb the surface of the eye, so you will not feel the laser pulses. What you may notice are bright flashes of light and possibly a slight sensation of pressure as the laser is applied, but these are not uncomfortable. The treatment is so quick that most patients are surprised at how straightforward it feels, with the entire laser process usually taking less than five minutes from start to finish.
5. Are there any serious risks?
Although YAG laser capsulotomy is very safe, no medical procedure is entirely risk-free. The most significant potential complication is retinal detachment, which occurs in a very small fraction of cases, usually in patients with high myopia or pre-existing retinal conditions. Other possible issues include a short-term rise in eye pressure, mild inflammation, or new floaters caused by debris in the vitreous gel. There is also a small chance of the artificial lens being marked by the laser, but this is rarely significant enough to affect vision. Your ophthalmologist will monitor you carefully after treatment to minimise these risks.
6. Will I still need glasses afterwards?
YAG capsulotomy restores clarity by removing the haze from the capsule, but it does not change the focusing power of your eye. If you needed glasses for reading, distance, or astigmatism before the capsule became cloudy, you will almost certainly still need them afterwards. What most patients notice, however, is that their glasses become effective again, since the blur caused by the capsule has been eliminated. In some cases, a small shift in prescription can occur, so your optometrist may suggest updating your lenses after the procedure.
7. Can everyone have YAG laser capsulotomy?
The majority of patients who develop posterior capsule opacification are suitable for YAG capsulotomy, but your ophthalmologist will confirm this with a full eye examination. Suitability depends on ensuring that PCO is truly the cause of your vision problems and not another underlying condition such as macular degeneration, glaucoma, or diabetic retinopathy. In rare cases, if the capsule has become very thick or fibrotic, the laser may be less effective, but this is uncommon. Most people with cloudy vision after cataract surgery are excellent candidates.
8. Does age affect the outcome?
Age plays a role mainly in the likelihood of developing posterior capsule opacification in the first place, rather than in how well the YAG treatment works. Younger patients tend to have more active lens cells, which means PCO can develop sooner after cataract surgery. However, once the capsule is cloudy, the effectiveness of YAG capsulotomy is the same for younger and older patients. Whether you are in your forties or your eighties, the laser procedure has an equally high chance of restoring clarity once the opacification is present.
9. How long does the procedure take?
The laser part of the treatment usually takes just a few minutes, but the full appointment is slightly longer. You’ll need time for your pupils to be dilated with drops, for the anaesthetic to take effect, and for checks both before and after the laser. In most clinics, you can expect to be there for about 30 to 45 minutes in total. Because there are no stitches or incisions, recovery is quick, and most people resume normal activities, including driving, the very next day.
10. Can YAG laser capsulotomy help with other eye problems?
No, this treatment is very specific. YAG capsulotomy only addresses the clouding of the posterior capsule that can occur after cataract surgery. If your vision problems are caused by other eye conditions such as macular degeneration, glaucoma, corneal disease, or diabetic changes in the retina, those will not improve with the laser. However, by clearing the haze from the capsule, YAG capsulotomy can make it easier to monitor and manage other conditions, since the view of the back of the eye becomes clearer for both you and your ophthalmologist.
Final Thoughts
YAG laser capsulotomy is one of the most successful and reliable procedures in ophthalmology. With success rates above 95%, quick recovery, and a low risk of complications, it offers a highly effective solution for the common problem of secondary cataracts.
If you’re struggling with cloudy vision after cataract surgery, it’s worth discussing YAG treatment with a specialist. To explore whether private cataract surgery at London Cataract Centre is right for you, book a consultation and get personalised advice tailored to your eyes.
References
- Apple, D.J., Solomon, K.D., Tetz, M.R., Assia, E.I., Holland, E.Y., Legler, U.F., Tsai, J.C. and Castaneda, V.E. (1992) ‘Posterior capsule opacification’, Survey of Ophthalmology, 37(2), pp. 73–116. doi:10.1016/0039-6257(92)90073-3. Available at: https://pubmed.ncbi.nlm.nih.gov/1455302/ (Accessed: 26 September 2025).
- Johansson, B., Lundström, M. and Montan, P. (2010) ‘Nd:YAG-laser capsulotomy rates in 3 × 300 eyes: five-year follow up of PCO incidence’, British Journal of Ophthalmology, 94(4), pp. 450–455. Available at: https://pubmed.ncbi.nlm.nih.gov/19828518/ (Accessed: 26 September 2025).
- Ursell, P.G., Spalton, D.J. et al. (2020) ‘5-year incidence of YAG capsulotomy and posterior capsule opacification after cataract surgery’, British Journal of Ophthalmology. Available at: https://pubmed.ncbi.nlm.nih.gov/31616057/ (Accessed: 26 September 2025).
- Lee, Y., Kim, J.S., Kim, B.G., Hwang, J.H., Kang, M.J. and Lee, J.H. (2023) ‘Comparison of the incidence of Nd:YAG laser capsulotomy based on the type of intraocular lens’, Medicina, 59(12), Article 2173. doi:10.3390/medicina59122173. Available at: https://doi.org/10.3390/medicina59122173 (Accessed: 26 September 2025).
- Wormstone, I.M. (2002) ‘Posterior capsule opacification: a cell biological perspective’, Experimental Eye Research, 74(3), pp. 337–347. doi:10.1006/exer.2001.1157. (Note: many journal platforms require institutional access for full text.)