If you’re living with chronic anaemia and need cataract surgery, it’s perfectly normal to feel a little anxious. After all, anaemia doesn’t just make you feel tired—it can affect how well your body handles stress, heals after surgery, and even responds to anaesthetic. But here’s the good news: with the right planning and support, you can still have a successful cataract procedure and enjoy clearer vision.
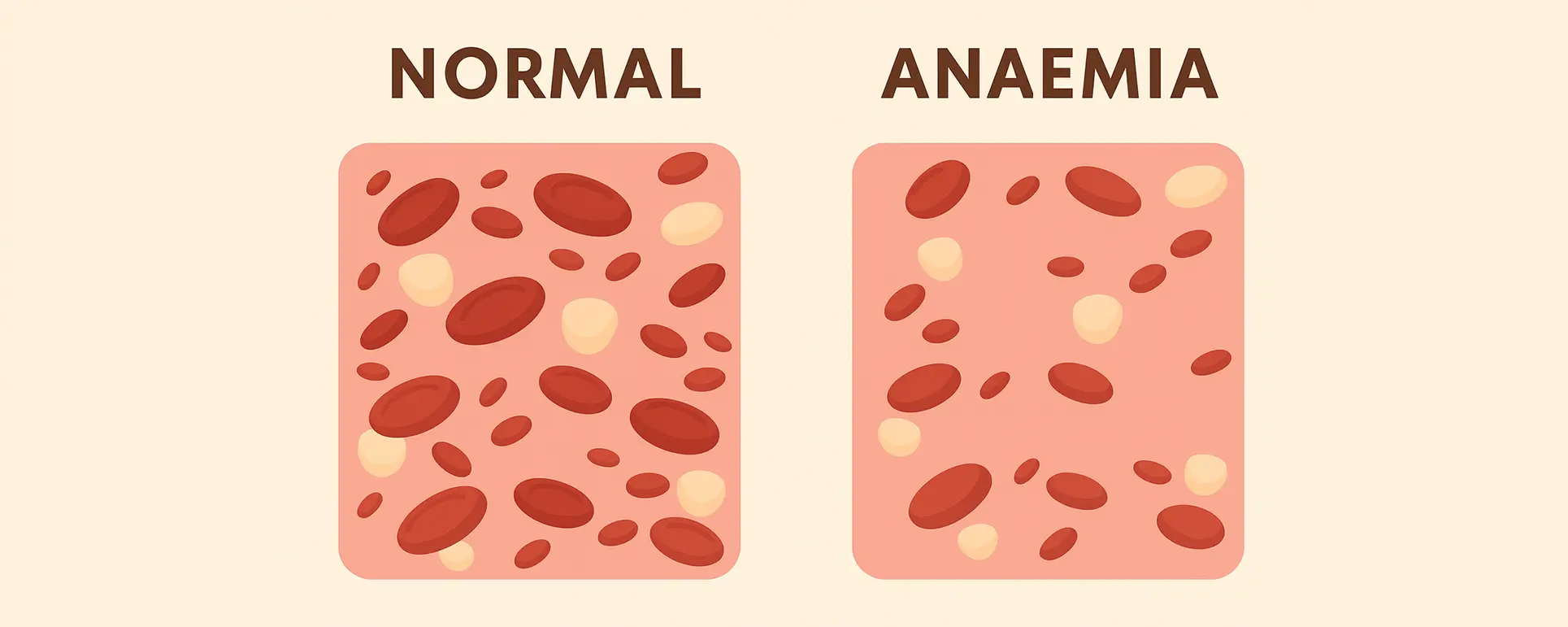
Anaemia means your red blood cells or haemoglobin levels are lower than normal, reducing the amount of oxygen your body can transport. This can impact everything from wound healing to your response to sedation. In cataract surgery—which is typically short and performed under local anaesthesia—these factors still need to be accounted for, especially if your anaemia is longstanding or caused by an underlying condition like kidney disease or autoimmune issues.
This guide walks you through how cataract surgery is managed in people with chronic anaemia—from pre-op planning to post-op recovery. It’s written with you in mind, so you feel confident and informed every step of the way.
Understanding Chronic Anaemia and Its Impact on Surgery
Chronic anaemia isn’t a condition to take lightly, especially when you’re considering surgery. Anaemia affects the oxygen-carrying capacity of your blood, which means your tissues and organs may not receive adequate oxygen during or after a procedure. This can influence everything from how your eye heals to how your body responds to anaesthesia, even if it’s just local.
The causes of chronic anaemia vary—some people have iron-deficiency anaemia that’s tough to correct, while others may have anaemia linked to kidney issues, bone marrow disorders, or long-term illnesses. Whatever the root cause, having a low haemoglobin baseline means your body is already operating with less reserve. That’s why your surgical team will take extra care to assess your fitness and optimise your health beforehand.
In practical terms, this might involve blood tests, a review of your medications, or even consultations with your GP or a haematologist before surgery. The aim is to make sure you’re in the best possible shape before undergoing your cataract procedure, and that all the right precautions are in place.
Preoperative Evaluation: Tailoring Your Plan

One of the most important steps in preparing for cataract surgery when you have chronic anaemia is a thorough preoperative evaluation. This isn’t just about checking your eye health—it’s a broader look at your systemic wellbeing. Your ophthalmologist may work closely with your GP or a haematologist to ensure that your haemoglobin levels are stable and that the cause of your anaemia is well understood.
You might be asked to do a full blood count, iron studies, and renal function tests before surgery. In some cases, additional steps like iron infusions or treatment for underlying conditions may be recommended ahead of the operation. If you’re already under the care of a specialist, sharing that information with your eye surgeon helps streamline the process.
Ultimately, the pre-op phase is about customising your care. You won’t be rushed into surgery. If your levels need to be optimised or stabilised first, your surgical date may be adjusted to ensure your body is in the best possible state to handle the procedure and recover smoothly.
Choosing the Right Anaesthetic Approach
Cataract surgery is usually done under local anaesthesia, often with a mild sedative. For most patients, this is straightforward. But if you have chronic anaemia, your anaesthetic plan may be adapted to reduce physiological stress and avoid triggering complications related to low oxygen levels.
Your surgical team will assess your oxygen saturation, pulse rate, and haemoglobin levels beforehand to ensure you’re stable. If you’re breathless or fatigued even at rest, a different anaesthetic approach might be considered—perhaps involving an anaesthetist in your care, even though cataract surgery doesn’t usually require general anaesthesia.
It’s also important that your team avoids medications that could interact negatively with your anaemia treatment, such as certain antibiotics or drugs that affect iron absorption. Tailoring the anaesthetic plan isn’t just about comfort—it’s about safety, especially when you’re working with limited physiological reserve.
Intraoperative Considerations: Minimising Surgical Stress

Although cataract surgery is a quick and minimally invasive procedure, your surgeon will still take extra steps to minimise stress on your body. That might include keeping the procedure as short and efficient as possible, using a well-controlled surgical environment, and closely monitoring your oxygen levels throughout.
Your cardiovascular status may be monitored more closely than usual, and supplemental oxygen might be provided if needed—even during a procedure that’s considered low-risk. The aim is to reduce any risk of hypoxia (low oxygen) which, in someone with anaemia, could pose a greater challenge.
Your eye itself will be handled gently to minimise inflammation and trauma, which could otherwise complicate recovery in people with compromised healing abilities. These adjustments are subtle, but together they make a significant difference when your body has to work harder to recover.
Recovery and Healing: What to Expect
After surgery, recovery is typically quick—but chronic anaemia can slow things down a little. You might take slightly longer to heal, and you may be more prone to fatigue during the first few days. However, serious complications are rare if you’ve had the right preparation and monitoring.
It’s important to keep up with your anaemia treatment during recovery—whether that’s iron supplements, folate, vitamin B12 injections, or other medication. Your GP may arrange follow-up blood tests to check your haemoglobin levels as you recover from surgery.
Post-op inflammation or infection can also be more problematic in people with immune-compromising conditions like anaemia of chronic disease, so be extra vigilant about your eye drops and hygiene. Don’t skip follow-up appointments, and let your clinic know if something doesn’t feel right.
Nutritional Support and Anaemia Management After Surgery
Your body needs nutrients to heal, and that’s especially true when you have anaemia. After cataract surgery, it helps to focus on a diet rich in iron, vitamin C, folate, and B12—all of which contribute to red blood cell production and tissue repair.
Foods like leafy greens, lean meat, lentils, nuts, eggs, and fortified cereals can support your recovery. If you’ve been advised to take supplements, keep going with them post-op unless your doctor says otherwise. Anaemia isn’t just about iron—it’s about your body’s overall ability to recover and regenerate, and food is a key part of that.
If your anaemia is linked to a chronic illness like kidney disease or an autoimmune disorder, sticking to your long-term treatment plan becomes even more important. Surgery recovery isn’t the time to let things slip—it’s when you need that extra bit of support to get your vision and energy back on track.
Risks and How They’re Managed
People with chronic anaemia may face a slightly higher risk of surgical complications—but the key word here is “slightly.” With proper planning and monitoring, most people go through cataract surgery with no major issues. However, it’s good to be aware of the potential risks so you can stay informed and proactive.
These risks may include delayed healing, increased susceptibility to infection, and more pronounced post-op fatigue. There’s also a very small risk that low oxygen delivery could affect eye tissue healing or worsen pre-existing eye conditions. But again, with a tailored approach, these risks can be minimised.
Your surgical team may advise additional follow-up visits, especially in the early stages of healing. If you experience unusual pain, blurry vision beyond the expected timeframe, or signs of infection, it’s important to act quickly. Early intervention can prevent a minor issue from becoming a major one.
The Role of Your GP or Haematologist in Surgical Planning

While your cataract surgeon is the main person performing the procedure, your GP and haematologist play a vital role behind the scenes. They help assess whether you’re fit for surgery, optimise your treatment plan, and support you before and after the operation.
In some cases, your GP may recommend a delay to surgery so your haemoglobin can be boosted, while your haematologist might tweak your anaemia medications to reduce risks during surgery. This collaborative approach is especially important in complex cases, like if you’re on erythropoietin injections or have transfusion-dependent anaemia.
Make sure all your doctors are in the loop. Bring your medication list to your pre-op appointments, and don’t hesitate to ask your surgeon to liaise with your other specialists. The more communication there is between teams, the safer and smoother your surgery experience will be.
FAQs About Cataract Surgery and Chronic Anaemia
- Can I have cataract surgery if my haemoglobin is low?
Yes, you can still have cataract surgery even if your haemoglobin is low, but your medical team may choose to delay the procedure slightly to improve your blood levels first. Surgery is generally safer when your haemoglobin is above a certain threshold, typically around 10 g/dL or higher, although this can vary depending on your overall health. If your anaemia is stable and not causing major symptoms like breathlessness or chest pain, cataract surgery under local anaesthetic can still go ahead with careful planning. Your surgeon will likely work with your GP or haematologist to make sure everything is well managed in advance. The goal is to reduce risks and help your body heal efficiently. - Will I need a blood transfusion before cataract surgery?
It’s unlikely you’ll need a blood transfusion specifically for cataract surgery, as the operation itself doesn’t involve significant blood loss. However, in cases of severe anaemia—especially if your haemoglobin is dangerously low or you’re showing symptoms of oxygen deprivation—your medical team might recommend a transfusion before surgery to stabilise your condition. This decision is usually made on a case-by-case basis, with input from a haematologist or your GP. The priority is ensuring your body has the capacity to cope with even minor surgical stress and to optimise post-op healing. In most patients, oral or intravenous iron therapy is sufficient. - Is the surgery more dangerous if I have anaemia?
There can be slightly increased risks when you have chronic anaemia, but cataract surgery remains one of the safest procedures available, even for people with underlying health conditions. The main concern is reduced oxygen delivery, which can affect tissue healing and resilience during recovery. However, with the right monitoring and preparation, the chances of complications remain very low. Your surgical team may take extra precautions such as using supplemental oxygen or scheduling closer follow-up appointments. Ultimately, the risk is manageable, and most patients with anaemia recover well after cataract surgery. - Will the anaemia affect my vision outcome?
Anaemia itself doesn’t directly impact the success of the artificial lens that’s implanted during cataract surgery. However, if your anaemia contributes to delayed wound healing or increases inflammation, it might temporarily affect how quickly your vision recovers. This is particularly relevant if your immune system is compromised or if you’re more prone to infections. That said, long-term visual outcomes are typically just as good in patients with anaemia, provided their condition is managed properly before and after surgery. Your surgeon will tailor your care plan accordingly to avoid complications that could slow your recovery. - Should I change my anaemia medication before surgery?
You shouldn’t make any changes to your anaemia treatment without speaking to your doctor first. In some cases, your GP or haematologist may adjust your medication or supplement regimen before the procedure—for example, if you’re taking iron tablets that cause gastrointestinal side effects or if you’re on erythropoietin injections that need to be timed differently. The idea is to keep your haemoglobin levels as steady as possible before surgery. Always bring a full list of your medications to your pre-operative appointment so your surgeon can check for any interactions or adjustments needed. - Can I go home the same day after cataract surgery?
Yes, cataract surgery is usually a day-case procedure, meaning you’ll go home the same day. Even if you have chronic anaemia, you won’t typically need to stay overnight unless there’s a specific concern flagged during your post-operative checks. You’ll rest for a short while after the surgery, during which the team will monitor your vital signs and make sure you’re stable. Provided you’re feeling well and there are no signs of dizziness, breathlessness, or fatigue that could pose a safety risk, you’ll be discharged with instructions and follow-up appointments in place. - What should I eat after surgery to support healing?
Your body needs extra support to heal properly, especially if you’re anaemic. Eating a nutrient-rich diet after surgery can make a noticeable difference to your recovery. Focus on iron-rich foods like spinach, red meat, lentils, and fortified cereals. Pair them with vitamin C sources such as citrus fruits or bell peppers to boost iron absorption. Don’t forget foods high in folate and vitamin B12, like eggs, dairy, and leafy greens, which are essential for red blood cell production. Maintaining a balanced, varied diet helps both your eye and body heal more efficiently after surgery. - Will I be more tired than usual after surgery?
It’s quite common for people with chronic anaemia to feel more fatigued than others after surgery, even when it’s a short procedure like cataract removal. Your body uses up energy to repair tissue and cope with surgical stress, and when oxygen delivery is reduced due to anaemia, this process can feel more draining. Make sure to rest as much as needed in the first few days after the operation. Avoid strenuous activity, stay hydrated, and ensure you’re getting enough nutrients. This period of fatigue should improve steadily as your body recovers and inflammation reduces. - Do I need to tell my surgeon if I have anaemia?
Yes, it’s very important to let your cataract surgeon know about your anaemia—even if it seems under control. Chronic anaemia can affect how your body responds to anaesthesia, how quickly you heal, and how your body copes with surgical stress. By being upfront, you allow your surgeon to put the right safety measures in place, such as liaising with your GP, scheduling closer monitoring, or adjusting your surgical timing. Omitting health details could increase your risk unnecessarily, so always share your full medical history during your pre-operative assessment. - How soon will I see better after the surgery?
Most people notice an improvement in their vision within a few days of cataract surgery, but if you have chronic anaemia, your recovery might take a little longer. That’s because your body may need more time to repair tissue, manage inflammation, and restore equilibrium. However, unless there are complications, you should still reach the same level of visual clarity as someone without anaemia—it may just require more patience. Staying on top of your post-op care and continuing with your anaemia treatment will help you heal steadily and enjoy long-term benefits from your cataract surgery.
Final Thoughts: Vision Is Possible—Even with Anaemia
At London Cataract Centre, we understand that living with chronic anaemia can make the idea of surgery feel a little daunting. But let us reassure you—having anaemia doesn’t mean you have to delay or miss out on the life-changing benefits of cataract surgery. What it does mean is that we need to approach your care with a little more planning, coordination, and personalisation.
Our team is experienced in managing complex medical cases, and we work closely with your GP, haematologist, and other specialists to ensure your cataract procedure is safe, smooth, and tailored to your health needs. From the first consultation to your final follow-up, we’re here to guide you every step of the way, with your wellbeing at the heart of everything we do.
References
1. Muñoz, M. et al. (2023) ‘Recommendations from the International Consensus Conference on patient blood management in surgery: identification and management of preoperative anaemia’, Annals of Surgery, 278(4), pp. 563–575. Available at: https://journals.lww.com/annalsofsurgery/fulltext/2023/04000/recommendations_from_the_international_consensus.8.aspx
2. Carson, J.L., Carless, P.A. and Hebert, P.C. (2015) ‘Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion’, Cochrane Database of Systematic Reviews, Issue 4, Art. No.: CD002042. Available at: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002042/full
3. Muñoz, M., Acheson, A.G., Bisbe, E., Butcher, A., Fullarton, G., Gómez‐Ramírez, S., et al. (2017) ‘International consensus statements on the management of postoperative anaemia after major surgical procedures’, Anaesthesia, 72(2), pp. 233–247. Available at: https://onlinelibrary.wiley.com/doi/abs/10.1111/anae.13747