If you’re preparing for cataract surgery and have dry eyes, you might be wondering whether this could affect the outcome. The truth is, it can—if it’s not properly identified and managed ahead of time. Dry eye doesn’t just cause irritation; it can also interfere with key surgical measurements, impact your healing, and affect how well your new lens implant performs.
The good news? Eye surgeons are well aware of this and have developed strategies to make cataract surgery safer and more successful for patients with dry eyes. Whether you’ve been formally diagnosed with dry eye or simply notice your eyes feel gritty or tired often, it’s worth understanding how this condition plays into your surgical journey.
In this article, we’ll walk through everything you need to know: from how dry eye is diagnosed and treated before surgery, to how to manage any post-op dryness, and when to speak up if your symptoms don’t improve.
What Is Dry Eye and Why Does It Matter?
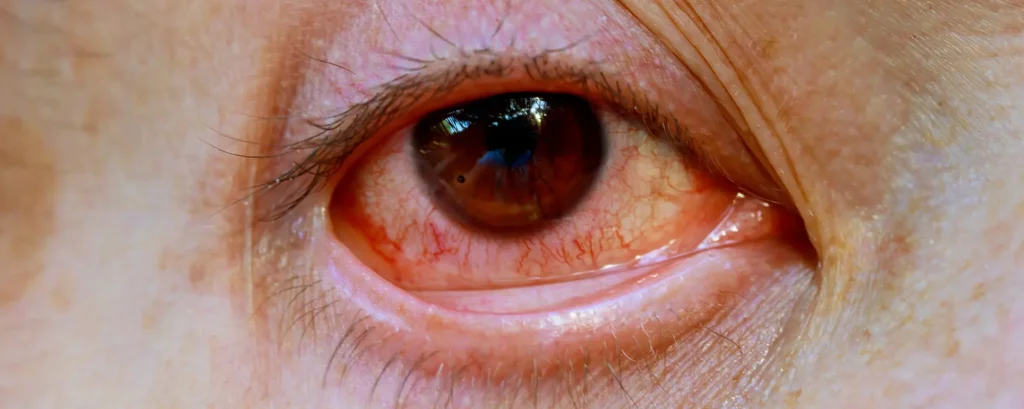
Dry eye occurs when your eyes don’t produce enough tears, or when the tears they do produce evaporate too quickly. This leads to a lack of proper lubrication on the surface of the eye, which can cause burning, itching, light sensitivity, blurry vision, and even eye fatigue.
When you’re having cataract surgery, your eye surgeon needs to take precise measurements of your cornea to select the right intraocular lens (IOL). If your eyes are dry, these measurements can be thrown off, leading to suboptimal visual outcomes. Dry eye can also increase inflammation after surgery and slow the healing process.
That’s why identifying and treating dry eye ahead of time is a key part of preparing for a smooth and successful cataract surgery.
Diagnosing Dry Eye Before Surgery
Most eye clinics now screen for dry eye as part of the pre-operative assessment. This might involve asking about symptoms, using special dyes to look at your tear film, or measuring tear production directly. Technologies like tear osmolarity tests and meibography (to assess the oil-producing glands in your eyelids) can give additional insight.
In many cases, patients don’t realise they have dry eyes until these assessments pick it up. That’s why it’s important to have a comprehensive pre-op exam that doesn’t just focus on your cataracts but looks at the whole health of your eye.
The aim of this evaluation is to catch any signs of dryness early, treat it before surgery, and get your eyes in the best shape possible to ensure accurate results.
How Dry Eye Can Affect Cataract Measurements
Accurate measurements are the foundation of successful cataract surgery. Your surgeon will assess the shape and power of your cornea using devices like keratometers and optical biometers. These tools rely on a stable, smooth tear film to deliver consistent results.
When the eye is dry, the tear film can break up quickly, leading to fluctuations in these readings. This can result in the wrong power of lens being chosen—especially if you’re getting a premium IOL like a toric or multifocal lens.
That’s why treating dry eye in advance isn’t just about comfort; it’s about ensuring the precision of your entire surgery plan.
Pre-Surgical Treatment for Dry Eyes

If dry eyes are identified during your pre-op assessment, your surgeon may delay surgery briefly to improve your ocular surface. This isn’t a setback—it’s an essential step to getting the best outcome.
Treatment might include artificial tears, prescription anti-inflammatory drops (like cyclosporine or lifitegrast), warm compresses, lid hygiene, omega-3 supplements, or in-office procedures like meibomian gland expression or punctal plugs.
Even a couple of weeks of treatment can significantly improve the tear film and make the eye surface more stable, ensuring better measurements and post-op healing.
What to Expect Post-Surgery if You Have Dry Eyes
It’s common for dry eye symptoms to temporarily worsen after cataract surgery. This can happen because the procedure disrupts the corneal nerves, reduces blink rate during recovery, and exposes the eye to antiseptics and light from the operating microscope.
You may notice increased burning, grittiness, or light sensitivity in the first few weeks. This is normal and usually settles as the eye heals.
Your surgeon will often continue or even increase your dry eye treatment during this time, so don’t be surprised if you’re using drops quite frequently after the operation.
Long-Term Management of Dry Eye After Cataract Surgery
For some people, cataract surgery can actually improve dry eye in the long run—especially if poor vision was making it harder to blink fully or care for the eyes. But for others, dryness may persist or require ongoing management.
This can include staying on artificial tears, maintaining good lid hygiene, avoiding environmental triggers, and using medications to reduce inflammation if needed. Regular follow-ups with your eye doctor are key.
It’s also important to be aware of other conditions that can overlap with dry eye, such as blepharitis or meibomian gland dysfunction, which might need separate treatments.
When to Seek Help for Persistent Symptoms
If you’re still experiencing dry eye symptoms three months after your surgery, it’s worth booking a follow-up appointment. You may need a reassessment of your treatment plan or testing for other conditions like ocular surface disease.
Don’t ignore symptoms like blurred vision that isn’t improving, persistent pain, or a feeling of something in your eye. These could indicate a more serious issue that needs prompt attention.
Good post-op care includes listening to your eyes and speaking up if something doesn’t feel right.
Supporting Your Eyes During Recovery: Practical Tips

There are simple things you can do to support healing if you have dry eyes after cataract surgery:
- Use preservative-free artificial tears regularly.
- Avoid staring at screens too long—remember to blink.
- Use a humidifier to reduce dry indoor air.
- Wear sunglasses outdoors to protect your eyes.
- Follow all prescribed medications strictly.
These habits help reduce strain, promote healing, and keep your eye surface comfortable while your vision settles.
Lifestyle Adjustments to Reduce Dry Eye Symptoms Long-Term
Even beyond the healing period, lifestyle changes can go a long way in managing dry eye. Hydration, diet, and environment all play a role.
Drinking plenty of water, eating foods rich in omega-3s (like salmon, flaxseeds, and walnuts), and avoiding excessive alcohol or caffeine can make a difference. Try to avoid direct fan or air conditioning blasts on your face.
If you wear makeup, go for hypoallergenic options and always remove it properly. Simple changes like these can improve tear film health and reduce flare-ups.
Choosing the Right IOL if You Have Dry Eye
If you’re considering premium lenses like multifocal or extended depth of focus IOLs, your surgeon will be especially careful with dry eye management.
These lenses rely on precise focusing, and dry eye can reduce their effectiveness. If your symptoms are severe or hard to manage, a monofocal lens may be recommended instead for more predictable clarity.
That said, many dry eye patients still do very well with premium lenses after stabilising their tear film first. It’s all about careful selection and individualised planning.
Frequently Asked Questions (FAQs)
- Can I still have cataract surgery if I have dry eyes?
Yes, you absolutely can. Having dry eyes doesn’t mean you can’t undergo cataract surgery, but it does mean your ophthalmologist will need to address the dryness before proceeding. This often involves using lubricating drops, treating any underlying eyelid inflammation, and allowing time for the ocular surface to improve. Once your tear film is more stable, your surgeon will be able to take more accurate measurements and ensure the surgery goes smoothly. - Will cataract surgery make my dry eyes worse?
It’s quite common for cataract surgery to temporarily worsen dry eye symptoms. This is usually due to the use of antiseptics, exposure to bright microscope lights, and the disruption of corneal nerves during the procedure. Most patients experience some increased dryness in the weeks following surgery, but this is generally short-lived and manageable with the right treatment plan, including preservative-free artificial tears and anti-inflammatory drops. - How is dry eye diagnosed before surgery?
Your eye clinic will carry out a number of tests during the pre-surgical assessment to detect dry eye. These can include questionnaires about your symptoms, slit-lamp examination with dye staining to observe the tear film, tear production tests such as Schirmer’s test, and imaging techniques like meibography to assess your eyelid glands. Diagnosing dry eye early helps tailor a treatment plan to improve the condition before surgery takes place. - How long before surgery should dry eye be treated?
In most cases, dry eye treatment should begin at least two to four weeks before surgery. This gives your eyes enough time to respond to therapy and for the tear film to stabilise. However, the exact duration depends on how severe your dry eye is and how quickly it improves. Your surgeon may choose to delay surgery slightly if they feel more time is needed to optimise your ocular surface. - Are premium lenses suitable for dry eye patients?
Premium lenses, such as multifocal and toric intraocular lenses, can still be an option for patients with dry eye, but only if the condition is well managed. These lenses require highly accurate measurements and a stable tear film to perform optimally. If your dry eye symptoms are severe or difficult to control, your surgeon may recommend a monofocal lens instead to avoid visual disturbances. The decision is always personalised based on your eye health and lifestyle goals. - What treatments are used for dry eyes before surgery?
A variety of treatments may be recommended to improve dry eye before surgery. These can include lubricating eye drops (especially preservative-free ones), anti-inflammatory medications like cyclosporine or lifitegrast, warm compresses to improve oil gland function, eyelid hygiene routines, omega-3 supplements, and sometimes punctal plugs to retain tears. In more severe cases, in-office procedures may be performed to express blocked glands. - What if my eyes are still dry months after surgery?
If you’re still experiencing dry eye symptoms several months after surgery, it’s important to return to your eye specialist for further evaluation. Persistent dryness could mean your initial treatment needs adjusting, or that there’s an underlying issue like blepharitis or ocular surface disease that hasn’t been addressed. Chronic dry eye is manageable, but it may require long-term care and a tailored treatment strategy to keep it under control. - Will treating my dry eyes improve my surgical outcome?
Yes, treating dry eye before surgery can significantly enhance the success of your cataract procedure. A stable tear film allows for more precise measurements, which helps your surgeon select the most accurate intraocular lens. It also reduces the risk of post-operative complications like inflammation or delayed healing. Managing dry eye is an essential step in ensuring you get the clearest and most comfortable vision after surgery. - Is dry eye more common after cataract surgery in older adults?
Yes, older adults are more prone to developing dry eye after cataract surgery. Ageing naturally leads to reduced tear production and changes in tear composition, which makes the eyes more vulnerable during and after procedures. Additionally, some older patients may already have undiagnosed meibomian gland dysfunction or eyelid issues that contribute to dryness. That’s why it’s crucial to screen for dry eye in all patients over 60 before surgery. - Can I do anything at home to help my dry eyes after surgery?
Definitely. There are several simple things you can do to support your eyes at home. Use preservative-free artificial tears regularly, especially if you’re spending time on screens. Keep your environment humidified, avoid direct exposure to fans or air conditioning, and wear sunglasses outdoors. Staying well-hydrated, eating a diet rich in omega-3s, and gently cleaning your eyelids each day can all make a noticeable difference to your eye comfort and recovery.
Final Thoughts
Dry eye is incredibly common in people over 60—and since that’s the age group most likely to need cataract surgery, it’s something every patient should be aware of. The key takeaway is this: cataract surgery is entirely possible with dry eyes, but it’s essential to manage the condition proactively.
By identifying and treating dryness ahead of time, maintaining good habits after surgery, and staying in touch with your eye care team, you give yourself the best chance of a smooth recovery and clear vision.
If you’re preparing for surgery and want to explore your options further, speak to a specialist at London Cataract Centre for tailored advice.
References
1. Miura, M., Inomata, T., Nakamura, M., Sung, J., Okumura, Y., Fujio, K., et al. (2022) ‘Prevalence and characteristics of dry eye disease after cataract surgery: a systematic review and meta-analysis’, Ophthalmology and Therapy, 11(4), pp. 1309–1332. Available at:
https://link.springer.com/article/10.1007/s40123-022-00513-y
2. Kawahara, A. (2024) ‘Management of dry eye disease for intraocular lens power calculation in cataract surgery: a systematic review’, Bioengineering, 11(6), article 597. Available at:
https://www.mdpi.com/2306-5354/11/6/597
3. Naderi, K., Gormley, J. and O’Brart, D. (2020) ‘Cataract surgery and dry eye disease: a review’, European Journal of Ophthalmology, 30(5), pp. 840–855. Available at:
https://journals.sagepub.com/doi/10.1177/1120672120929958
4. Collaborative Eye Editorial Board (2020) ‘Treat dry eye disease before cataract and refractive surgery’, Collaborative Eye, October. Available at:
https://collaborativeeye.com/articles/2020-oct/treat-dry-eye-disease-before-cataract-and-refractive-surgery/

