If you’ve been diagnosed with myelodysplastic syndrome (MDS) and now need cataract surgery, you might have some understandable concerns. MDS affects your bone marrow and blood cell production — and that means your immune system, clotting ability, and healing response may not be quite the same as someone without the condition. But that doesn’t mean you can’t have cataract surgery. It just means your surgeon and haematologist need to take a few extra steps to ensure everything goes as safely and smoothly as possible.
In this guide, we’ll walk you through exactly what to expect — from pre-op blood tests and infection risk assessments to anaesthesia choices and aftercare. The goal is to demystify the process and show you how the right precautions can make a real difference to outcomes. Cataracts can have a major impact on your vision and quality of life — and having MDS shouldn’t stop you from seeing clearly again.
Understanding Myelodysplastic Syndrome and Its Impact on Surgery
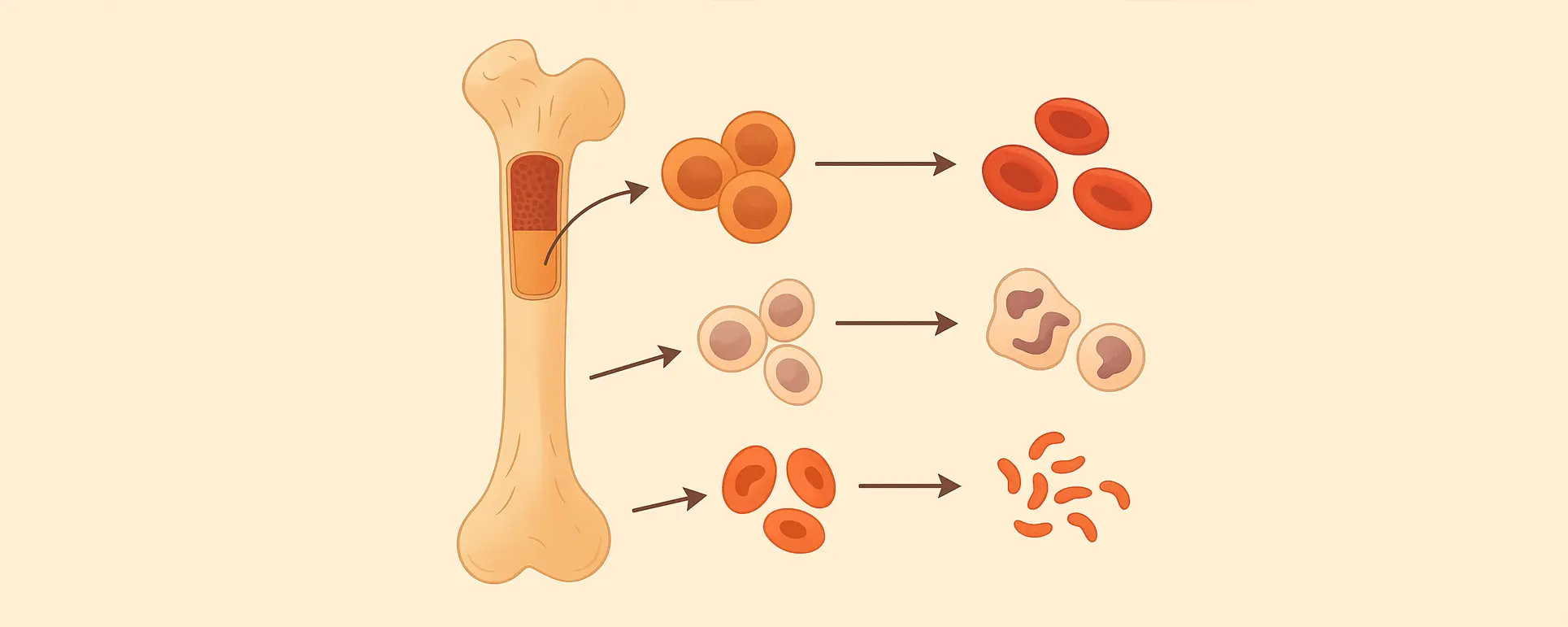
Let’s start with the basics. Myelodysplastic syndrome is a group of disorders where your bone marrow doesn’t produce blood cells properly. That includes red blood cells (which carry oxygen), white blood cells (which fight infection), and platelets (which help your blood clot). People with MDS often have one or more of these cell types running low — which doctors refer to as cytopenias.
So, how does this affect surgery? First, low white cell counts can raise your infection risk. Second, if your platelets are too low, there’s a higher risk of bleeding. And third, if your red cells are too low, you might feel fatigued or even dizzy from low oxygen levels. All of these factors need to be taken into account when planning any procedure — even something as minimally invasive as cataract surgery.
Luckily, modern eye surgery is very refined. Cataract removal is typically done with tiny instruments, under local anaesthetic, and doesn’t involve large incisions. That makes it a lot safer for people with blood disorders — as long as we check the right things beforehand and plan your care around your unique situation.
Preoperative Planning: The Role of Your Haematologist

Before any decision is made about going ahead with cataract surgery, your ophthalmologist will likely want to talk to your haematologist. That’s because your haematologist knows your blood counts best — and can advise if you need a blood transfusion, platelet support, or antibiotics before surgery.
In many cases, a full blood count (FBC) will be done a few days or weeks before the procedure. If your white cell count is too low, you may be given medications like G-CSF to stimulate production. If your platelets are below a safe threshold — usually around 50,000 per microlitre — a transfusion may be recommended just before the surgery.
This kind of preparation can make a big difference. It turns a higher-risk situation into a manageable one. And when your eye surgeon and haematologist work together, they can create a care plan that puts your safety first while still restoring your vision.
Choosing the Right Type of Anaesthesia
Anaesthesia is another key consideration. Most cataract operations in the UK are done with local anaesthesia — either as drops, a small injection around the eye, or a combination of both. This means you stay awake during the procedure but feel no pain. It also avoids the risks of general anaesthesia, which is especially useful if you have other health issues linked to MDS.
For patients with severe anxiety or tremor, light sedation may also be offered. But this needs to be carefully balanced with your overall health status. Your medical team will assess your cardiovascular fitness and blood oxygen levels before making a decision.
The good news is that most people with MDS can tolerate local anaesthetic cataract surgery very well. And since you’ll be going home the same day, the overall stress on your system is kept to a minimum.
Managing the Risk of Bleeding
One of the most important factors for your surgical team to manage is your platelet count. Platelets are essential for blood clotting. In MDS, some people experience thrombocytopenia (low platelets), which can make even small procedures riskier in terms of bruising or bleeding.
Before surgery, your platelet level will be checked. If it’s below the safe range (usually <50,000), your haematologist may recommend a platelet transfusion. This might be given on the morning of surgery or even a day before, depending on logistics and how fast your body uses up transfused platelets.
The eye itself doesn’t have large blood vessels where cataract surgery is performed, but even a tiny bit of bleeding can cloud your view during or after the operation. That’s why it’s always better to optimise your clotting profile ahead of time.
Infection Prevention: A Key Priority
Having a lower white cell count means your body might not fight off infections as effectively. That makes infection prevention a top priority when planning cataract surgery in someone with MDS.
The eye is thoroughly cleaned with antiseptic before surgery, and antibiotics may be used in two ways: as drops before and after surgery, and/or injected directly into the eye at the end of the procedure (a method known as intracameral antibiotics). This has become a standard practice in many hospitals to prevent endophthalmitis, a rare but serious eye infection.
In some cases, your haematologist may suggest additional systemic antibiotics if your neutrophil count is very low or if you’re already on prophylactic medication. This extra layer of care helps prevent infections from gaining a foothold in the days after surgery.
What to Expect During Cataract Surgery

Cataract surgery itself is quick — usually taking about 15 to 30 minutes. You’ll be lying down, and the surgeon will use a microscope to look into your eye while they work. Most operations are done using phacoemulsification, where ultrasound breaks up the cloudy lens before it’s removed and replaced with a clear artificial lens.
Throughout the procedure, your blood pressure and oxygen levels will be monitored. If you’re prone to low blood pressure or oxygen due to MDS-related anaemia, the surgical team will have oxygen and support available.
Once the surgery is complete, you’ll rest for a short while and then be discharged home with instructions and eye drops. Your follow-up visit is usually within 24–48 hours to check healing and vision.
Recovery and Aftercare: Special Considerations
Post-operative care after cataract surgery in someone with MDS doesn’t look wildly different from the standard protocol — but a few extra precautions are in place. You’ll likely be given antibiotic and steroid eye drops to prevent infection and reduce inflammation. But you may also be asked to monitor more closely for signs of infection, such as redness, discharge, or pain.
You might be seen more frequently than other patients, especially if your white cell count is very low. This allows the surgeon to catch any problems early and act fast. If your vision suddenly worsens, or the eye becomes very sore, don’t wait for your next appointment — you should be reviewed urgently.
It’s also important to avoid heavy lifting, bending, or touching your eye. If you experience fatigue due to anaemia, take extra care not to strain yourself during recovery. Most people feel back to normal within a week or two, and vision often improves dramatically even within the first few days.
When Cataract Surgery Might Be Delayed
Sometimes, it’s safer to wait. If your blood counts are unstable, your haematologist may advise postponing surgery until things are better controlled. For example, if you’ve recently had a bone marrow transplant, a hospital admission, or an episode of sepsis, you may need more time to recover before an elective procedure.
Your surgeon will also assess how urgently the cataract needs removing. If your vision is only mildly reduced and you’re managing daily life well, it may be worth deferring surgery for a while. On the other hand, if the cataract is advanced and affecting your safety or independence, your care team may find ways to move ahead with the right precautions.
Every decision is made on a case-by-case basis — with your safety, eyesight, and long-term health in mind.
The Psychological Side: Addressing Worry and Uncertainty
Living with MDS is already a challenge, and facing surgery can stir up a lot of worry. You may be anxious about complications, tired from ongoing treatments, or simply unsure whether it’s worth it. These feelings are valid — and it’s important to raise them with your medical team.
Many eye clinics now offer pre-assessment counselling, where you can talk through any concerns. Understanding the process — and knowing you’re not alone — can ease anxiety and help you feel more confident in your decision.
Support from family, friends, or an MDS charity group can also be a big source of strength during this time.
FAQs About Cataract Surgery and Myelodysplastic Syndrome (MDS)
- Is cataract surgery safe if I have low platelets?
Cataract surgery can still be performed safely in people with low platelets, but only with the right precautions. Your haematologist will check your most recent platelet count and, if necessary, arrange a platelet transfusion before the procedure to reduce the risk of bleeding. The surgery itself involves minimal trauma and only very small incisions, so with proper planning, the bleeding risk can be well controlled. - Will I need to stop any medications before surgery?
You may be advised to adjust or pause certain medications before cataract surgery, particularly if you’re taking blood thinners or immunosuppressants. However, this decision will be made jointly by your haematologist and ophthalmologist, as stopping some treatments too soon could pose other risks. Always inform your surgical team of every medication and supplement you take, including herbal remedies. - Can I have cataract surgery while on azacitidine or other MDS treatments?
It depends on how well your blood counts are being managed and whether you’re experiencing side effects from treatment. In many cases, cataract surgery can be timed between treatment cycles or scheduled when your blood counts are most stable. Your medical team will assess the risks and benefits and may suggest brief adjustments to your treatment schedule if needed. - Will I need to stay in hospital overnight?
Most people with MDS are still able to have cataract surgery as a day case, meaning you go home the same day. However, in rare cases — such as if your blood counts are very unstable or you live far from the hospital — an overnight stay may be recommended for closer monitoring. Your team will make this decision based on your individual circumstances. - How soon will my vision improve?
Many people begin to notice clearer vision within 24 to 72 hours after cataract surgery, though recovery speed can vary. If you have fatigue, anaemia, or inflammation related to MDS, your recovery might be slightly slower. Nonetheless, the majority of patients with MDS still experience excellent visual outcomes after surgery with proper aftercare. - Are there any long-term risks to having cataract surgery with MDS?
There are no specific long-term risks caused by MDS itself, but people with this condition may be slightly more prone to post-operative infections or slower healing. These risks are usually well managed by using antibiotic drops, close follow-up, and collaboration between your ophthalmologist and haematologist. Most patients recover fully without complications. - What if I need cataract surgery in both eyes?
If both eyes are affected, your surgeon will usually operate on one eye first and allow time for it to heal before addressing the second. This staged approach gives your team a chance to assess how well your body responds to the first surgery, which is especially helpful when managing a condition like MDS. - Can MDS cause cataracts to form?
MDS itself doesn’t directly cause cataracts, but some of the treatments used — such as corticosteroids or chemotherapy — can accelerate cataract development over time. Age is still the most common cause, but having MDS can increase the likelihood of needing cataract surgery a bit earlier than expected. - Should I tell the eye clinic about all my medications?
Yes, it’s absolutely essential. You should give your ophthalmologist a full list of everything you take, including prescribed drugs, over-the-counter medicines, and supplements. This helps your team plan anaesthesia, assess bleeding or infection risk, and avoid any drug interactions that could affect your surgery or recovery. - What signs should I watch for after surgery?
After cataract surgery, look out for any signs of infection or inflammation, such as increasing redness, pain, blurred vision, discharge, or sensitivity to light. If you notice any of these symptoms, contact your eye clinic immediately — prompt treatment can prevent complications and protect your vision.
Final Thoughts
Cataract surgery in people with myelodysplastic syndrome might require a few extra steps, but it’s absolutely possible — and often well worth doing. The key is teamwork. Your eye surgeon, haematologist, and you all play a role in ensuring a smooth, safe experience.
At London Cataract Centre, we’re experienced in managing complex medical cases like MDS, and we work closely with your wider healthcare team to tailor every aspect of your care. From preoperative planning to postoperative follow-up, our focus is on providing safe, effective surgery that restores your vision without compromising your overall health.
If your eyesight is starting to interfere with your daily life, don’t assume you have to just live with it. With the right checks, timing, and collaboration, cataract surgery can be done successfully — even with a condition as complex as myelodysplastic syndrome.
References
- Lombard, F.W., Popescu, W.M. & Kertai, M.D., 2021. Perioperative thrombocytopenia: evidence, evaluation, and emerging therapies. Current Opinion in Anaesthesiology, 34(3), pp.335–344. Available at: https://pubmed.ncbi.nlm.nih.gov/33935182/ [Accessed 23 July 2025]
- Estcourt, L.J. et al., 2018. Prophylactic platelet transfusions prior to surgery for people with a low platelet count. Cochrane Database of Systematic Reviews, (9):CD012779. Available at: https://pubmed.ncbi.nlm.nih.gov/30221749/ [Accessed 23 July 2025]
- Stanworth, S.J. et al., 2015. Risk of bleeding and use of platelet transfusions in patients with haematologic malignancies. Haematologica, 100(6). Available at: https://haematologica.org/article/view/7404 [Accessed 23 July 2025]
- International Haematological Society, 2018. Perioperative thrombocytopenia: recommended approaches for safe surgery. British Journal of Anaesthesia. Available at: https://www.bjanaesthesia.org.uk/article/S0007-0912(18)30753-0/pdf [Accessed 23 July 2025]