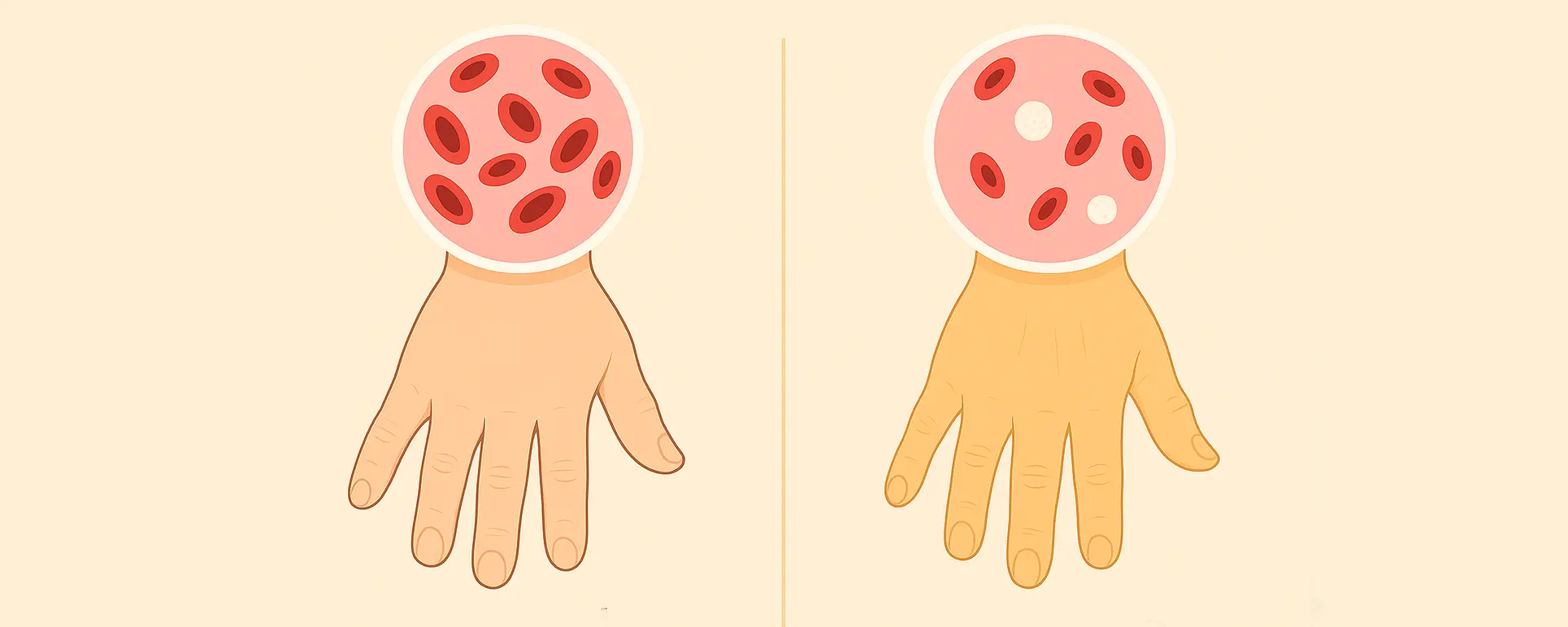
It might surprise you to learn that sickle cell disease can directly affect your vision. The abnormal red blood cells can block tiny blood vessels in the eye, leading to various complications. These include conditions like sickle cell retinopathy, which can cause bleeding, scarring, or even retinal detachment if left untreated. The reduced oxygen supply to the eye’s tissues can also result in damage to the optic nerve or other delicate structures.
Over time, chronic low oxygenation can speed up the development of cataracts. In fact, certain medications used to manage sickle cell crises — particularly corticosteroids — can also increase your risk of cataracts. For some patients, this means developing cataracts earlier in life than would be typical.
So, if you’re noticing blurry vision, increased glare, or trouble seeing at night, don’t assume it’s just part of your sickle cell symptoms — it might actually be a treatable cataract. The key is catching it early and discussing your options with an experienced eye surgeon who understands the unique needs of patients with sickle cell anaemia.
Are Cataracts More Common in People with Sickle Cell Anaemia?
Yes, they are. While cataracts usually develop as part of the natural ageing process, people with sickle cell disease are at a higher risk of developing them at a younger age. There are several reasons for this increased risk.
Firstly, as we mentioned, the reduced oxygen flow to the eye can accelerate cataract formation. Secondly, repeated sickling crises and chronic inflammation can contribute to damage in the eye’s lens. Thirdly, if you’ve been treated with steroids — either for managing sickle cell complications or other autoimmune issues — this medication is known to cause or speed up the formation of posterior subcapsular cataracts.
So, while you might be focused on managing your systemic symptoms, it’s crucial not to neglect regular eye checks. Early diagnosis means a wider range of treatment options — and potentially a better outcome.
Preoperative Planning: It Starts with Your Haematologist

Cataract surgery may be quick and straightforward for most people, but if you have sickle cell anaemia, preparation is everything. Your eye surgeon won’t go ahead without liaising with your haematology team first. Why? Because your systemic health plays a direct role in how well you’ll tolerate the surgery.
Your blood count, haemoglobin levels, and history of crises are all considered before giving the green light. In some cases, your haematologist may recommend a blood transfusion before the operation to reduce the risk of sickling during the procedure. This step ensures your blood can carry enough oxygen and decreases the chance of blockage in tiny vessels.
Hydration and oxygenation are critical, too. You’ll be encouraged to stay well-hydrated, and supplemental oxygen may be used during the procedure, even if it’s performed under local anaesthetic. All of this is done to minimise any risk of triggering a sickling crisis.
Anaesthesia Choices: Local Over General (In Most Cases)
When it comes to anaesthesia for cataract surgery, local anaesthetic is generally the safer choice for patients with sickle cell anaemia. That’s because general anaesthesia carries a slightly higher risk of reducing oxygen levels in your body, which can trigger sickling.
With local anaesthetic, only the eye area is numbed — meaning you stay awake, your breathing stays regular, and your risk of complications is lower. Most modern cataract procedures are done this way, using eye drops or a small injection to numb the area. In rare situations, if a general anaesthetic is unavoidable (for example, in children or patients with extreme anxiety), your care team will take additional precautions to manage your oxygen levels and keep your body temperature stable.
The anaesthetist will be fully briefed on your condition and may administer extra fluids and oxygen to prevent dehydration or hypoxia. It’s all about creating a controlled environment where your risk of a sickling crisis is brought down to nearly zero.
Surgical Technique: Precision and Speed Matter

Cataract surgery in sickle cell patients is performed with the same precision and technique as any other case, but the focus on reducing surgical stress is even greater. The operation itself typically involves making a tiny incision in the eye, breaking up the cloudy lens using ultrasound (a process called phacoemulsification), and replacing it with a clear artificial lens.
In your case, the surgeon may aim to complete the procedure slightly faster than average, without compromising safety. The reason? The longer the eye is exposed and the longer you’re under the surgical drapes, the higher the chance of stress to your body — which can affect your blood flow.
Intraocular pressure is carefully monitored, and medications may be used during surgery to control inflammation or reduce the chance of complications post-op. Everything is tailored to make the experience as smooth and low-risk as possible.
Postoperative Recovery: What’s Different?
The recovery process after cataract surgery is usually straightforward, but in patients with sickle cell anaemia, there are a few added precautions. Firstly, you’ll be monitored more closely in the first few hours after surgery to ensure there are no signs of a crisis or complications. You may be advised to rest in a slightly upright position and avoid bending over, which could increase pressure in the eye.
Your medications will also be carefully managed. For instance, anti-inflammatory eye drops are standard after surgery, but if you’re already on systemic medications or steroids, the doses may need adjusting to avoid conflicts. Pain management is important too — not just for comfort, but because severe pain can actually trigger a sickling episode. Your doctor will work with you to make sure you stay comfortable without compromising safety.
In the days and weeks after surgery, your eye will gradually heal, and you should notice improved clarity and reduced glare. Just be sure to keep all follow-up appointments and report anything unusual — like pain, reduced vision, or redness — immediately.
Coordination with Your Medical Team
The best outcomes in cataract surgery for sickle cell patients come from a team approach. That means your ophthalmologist, haematologist, GP, and possibly a specialist nurse will all be involved. This ensures nothing is missed — from pre-surgery blood work to postoperative pain management.
You’ll also be encouraged to keep up with your regular sickle cell monitoring during this period. If any signs of infection, dehydration, or stress arise, prompt intervention can prevent complications. Remember, it’s not just about the surgery — it’s about managing your overall health throughout the process.
Special Considerations for Children and Teens with SCD

If the patient needing cataract surgery is a child or teenager with sickle cell disease, the planning becomes even more intricate. Cataracts in younger patients with SCD can develop due to steroid use or complications from previous eye inflammation. But paediatric surgery often requires general anaesthesia, which comes with extra risks in these cases.
In such scenarios, a paediatric anaesthetist experienced with SCD is essential. The surgery will be timed to avoid any recent sickle cell crises, and blood transfusions may be scheduled in advance. Parents should be fully informed about all the steps involved — from pre-op fasting to post-op follow-up care.
While recovery is often quick in younger patients, the need for long-term monitoring is even greater. Children may require additional support for visual development, including glasses or vision therapy if the cataract had been present for a long time before surgery.
Setting Realistic Expectations for Vision
This is an important one: not everyone with sickle cell disease who has cataract surgery will end up with perfect vision. If your eyes have already been affected by sickle cell retinopathy, optic nerve damage, or previous inflammation, the clarity of vision you achieve post-surgery might be limited.
That said, removing the cataract can still provide a big improvement in your quality of life. Even if you don’t regain 20/20 vision, you may notice brighter colours, less glare, and better focus. That’s why it’s so important to have a detailed discussion with your surgeon before the operation to understand what results are realistically achievable in your specific case.
FAQ: Cataract Surgery and Sickle Cell Anaemia
- Can people with sickle cell anaemia safely have cataract surgery?
Yes, people with sickle cell anaemia can safely have cataract surgery when the procedure is properly planned in advance and coordinated with a haematologist. The surgical team will take specific precautions to prevent sickling crises, such as ensuring adequate oxygenation, hydration, and temperature control throughout. The key to safety is a personalised approach that accounts for your overall health and medical history, making the operation just as successful as in patients without sickle cell disease. - Why is sickle cell anaemia a concern during eye surgery?
Sickle cell anaemia can increase the risk of complications during surgery because the abnormal red blood cells are more likely to block small blood vessels when exposed to stress, low oxygen levels, or dehydration. Even though cataract surgery is usually low risk, these triggers can be present in the surgical environment if not managed carefully. This is why patients with sickle cell anaemia need tailored precautions to avoid painful and potentially dangerous sickling events before, during, and after surgery. - Will I need a blood transfusion before cataract surgery?
Some patients with sickle cell anaemia may require a blood transfusion before cataract surgery to reduce the percentage of sickled cells and increase the amount of healthy haemoglobin in the bloodstream. This helps to improve oxygen delivery and reduces the risk of complications during the procedure. The decision to perform a transfusion will be made by your haematologist in collaboration with your eye surgeon, based on your haemoglobin level, medical history, and current state of health. - Is local or general anaesthesia better for patients with sickle cell disease?
Local anaesthesia is generally preferred for cataract surgery in patients with sickle cell disease because it avoids the respiratory risks associated with general anaesthesia and helps maintain stable oxygen levels. Keeping the patient awake during surgery also makes it easier to monitor for signs of distress or discomfort. However, in rare cases where local anaesthesia isn’t appropriate — such as with extreme anxiety or in children — general anaesthesia may still be used with additional safeguards in place. - Can sickle cell anaemia cause cataracts?
Yes, people with sickle cell anaemia are more likely to develop cataracts earlier in life due to a combination of reduced oxygen supply to the eye, chronic inflammation, and side effects of long-term medications like corticosteroids. These factors can cause damage to the lens of the eye over time, leading to clouding and visual impairment. Cataracts in sickle cell patients often develop more rapidly than in the general population, so regular eye checks are essential to detect them early. - Will cataract surgery fix all my vision problems?
Cataract surgery will remove the cloudy lens and can significantly improve vision clarity, but it won’t resolve other eye issues caused by sickle cell disease, such as sickle cell retinopathy or optic nerve damage. If you’ve already experienced complications in the retina or back of the eye, your overall visual outcome may be more limited. Still, many patients with sickle cell disease benefit greatly from surgery, even if the improvement isn’t total, because clearer vision can make daily life much easier. - How long does recovery take after cataract surgery with sickle cell anaemia?
Recovery from cataract surgery typically takes a few weeks, but patients with sickle cell anaemia may require closer observation during this period to monitor for signs of complications like pain, inflammation, or sickling events. You’ll be prescribed eye drops to manage inflammation and prevent infection, and your medical team may continue to support you with hydration and oxygen if needed. Most patients can return to their usual activities fairly quickly, provided they follow their aftercare instructions closely. - What precautions are taken during the surgery to prevent a crisis?
Several precautions are taken during cataract surgery to reduce the risk of a sickle cell crisis, including maintaining a warm environment, ensuring the patient is well hydrated, supplying oxygen if necessary, and minimising surgical stress. The anaesthetist monitors oxygen saturation and vital signs throughout, and the surgeon uses gentle, efficient techniques to keep the procedure brief and low-risk. These steps are all designed to create a stable environment that prevents red blood cells from sickling. - Do I need to stop my sickle cell medications before surgery?
In most cases, patients with sickle cell anaemia do not need to stop their regular medications before cataract surgery, but your medical team will review everything you’re taking to make sure it’s safe to continue. Some drugs may be temporarily adjusted to reduce risk during the perioperative period, especially if you’re on hydroxyurea, steroids, or pain management medications. Always follow your doctor’s advice and never stop any medication without explicit medical guidance. - Where should I go for cataract surgery if I have sickle cell anaemia?
If you have sickle cell anaemia, it’s important to choose a cataract surgery provider experienced in managing patients with complex medical conditions. Specialist clinics like London Cataract Centre are well-equipped to coordinate care with your haematologist, take extra precautions during surgery, and provide the necessary post-operative support to reduce your risks and maximise your visual outcome. Having the right team in place makes all the difference to your safety and recovery.
Final Thoughts: It Can Be Done — and Safely
If you have sickle cell anaemia and are worried about cataract surgery, you’re not alone. But with the right precautions, experienced clinicians, and a coordinated approach, the procedure is not only safe — it can dramatically improve your daily life. Don’t let fear hold you back from exploring an option that could restore your vision and independence.
At London Cataract Centre, we regularly treat patients with complex medical backgrounds, including those with sickle cell anaemia. We work closely with haematologists and tailor every aspect of the procedure to suit your individual needs. Your safety, comfort, and visual outcome are our top priorities.
References
- Adjepong, K.O., Otegbeye, F. and Amoateng-Adjepong, Y. (2018) ‘Perioperative management of sickle cell disease: A narrative review’, Mediterranean Journal of Hematology and Infectious Diseases, 10(1), e2018.032. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7586501/ (Accessed: 17 July 2025)
- AlRyalat, S.A. et al. (2020) ‘Ocular manifestations of sickle cell disease: Signs, symptoms and complications’, Ophthalmic Epidemiology, 27(4), pp. 259–264. Available at: https://pubmed.ncbi.nlm.nih.gov/32013659/ (Accessed: 17 July 2025)
- OpenAnesthesia (2024) ‘Sickle cell disease: perioperative management’, OpenAnesthesia. Available at: https://www.openanesthesia.org/keywords/sickle-cell-disease-perioperative-management/
- Association of Anaesthetists (2021) ‘Guideline on the peri‑operative management of patients with sickle cell disease’, Anaesthesia. Available at: https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/10.1111/anae.15349 (Accessed: 17 July 2025)
- Taylor, C. et al. (2024) ‘Proliferative sickle cell retinopathy: A patient and a physician’s perspective on quality of life and quality of eye care’, Ophthalmology and Therapy, 13, pp. 851–860. Available at: https://doi.org/10.1007/s40123-024-00893-3 (Accessed: 17 July 2025)