If you’re living with liver cirrhosis and have been told you need cataract surgery, it’s natural to have a few questions. How safe is the procedure in your case? Will your liver condition make things more complicated? And what should your surgeon be looking out for? In this article, we’re going to unpack all of that – from how cirrhosis affects blood clotting to why healing might take longer, and what your eye surgeon and anaesthetist can do to keep you safe.
Understanding Liver Cirrhosis and Why It Matters in Cataract Surgery
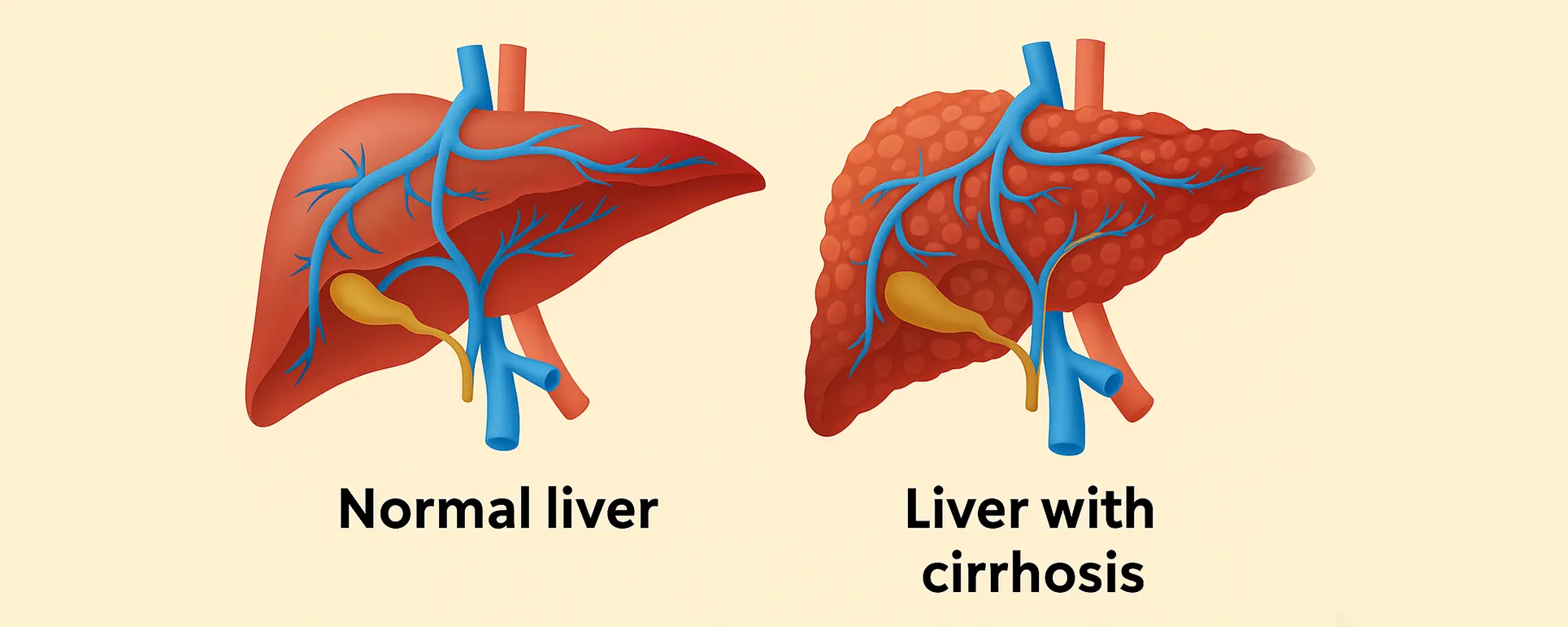
Cirrhosis is a condition where the liver gradually becomes scarred and loses its ability to function properly. This can affect various systems in your body – including how well your blood clots, how your body processes medications, and how quickly you heal after surgery. And while cataract surgery is typically a low-risk outpatient procedure, cirrhosis introduces a few extra layers of complexity.
Liver disease alters the balance of clotting and anti-clotting factors in your blood. In addition, your liver plays a central role in metabolising medications – including the sedatives and antibiotics used during eye surgery. That means even routine medications might linger longer in your system, causing side effects or complications.
But the good news? With the right precautions, cataract surgery can still be performed safely and effectively in people with cirrhosis. Let’s take a closer look at what that involves.
Coagulation Risks: The Bleeding Edge of Liver Cirrhosis
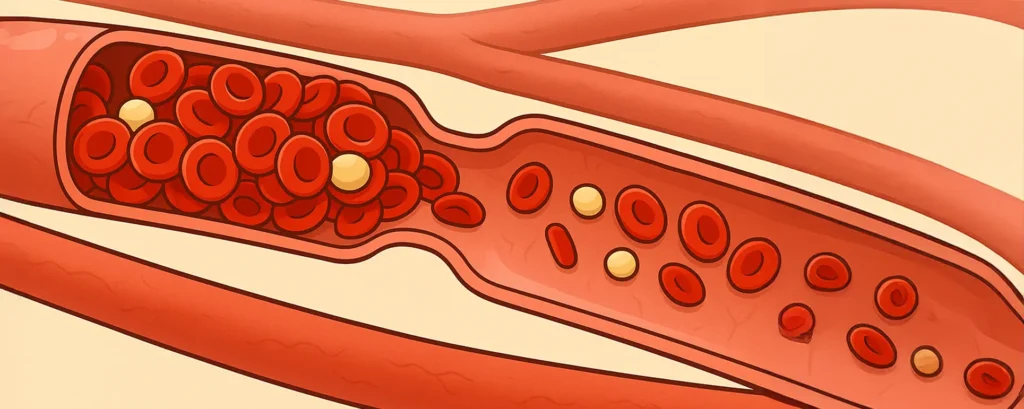
One of the liver’s many jobs is to produce proteins that help your blood clot. When it’s not working properly, you’re more prone to bleeding – and even minor trauma, like a surgical incision in the eye, can sometimes result in more bruising or haemorrhage than expected.
Monitoring Your INR and Platelet Count
Before cataract surgery, your surgeon and anaesthetist will want to check two key things: your INR (International Normalised Ratio) and your platelet count. A high INR means your blood takes longer to clot, which increases bleeding risk. A low platelet count – also common in cirrhosis due to spleen enlargement – further adds to the problem.
If your INR is mildly elevated, you may still be able to proceed with surgery, but with extra care. For significantly raised levels, you might need vitamin K supplementation or even a temporary correction using clotting factors or plasma. Platelet transfusions might be necessary if counts are critically low.
Local Anaesthesia vs General: A Safer Bet?
In most cases, cataract surgery can be performed under local anaesthesia using eye drops or a small injection around the eye. This approach reduces the bleeding risk that comes with general anaesthesia, especially in patients with varices or portal hypertension. It also avoids the need for airway manipulation, which could be risky in patients with coagulopathy.
Surgeons often choose minimally invasive techniques and ensure that any small vessels around the conjunctiva are gently cauterised to prevent unnecessary bleeding. A careful, no-touch approach goes a long way in cirrhotic patients.
The Anaesthesia Challenge: Liver Metabolism and Sedative Sensitivity

One of the biggest considerations in cirrhosis is how your body handles anaesthetic drugs. The liver is the main hub for metabolising most sedatives, analgesics, and anti-nausea medications. When it’s compromised, drugs can stay in your system longer, leading to prolonged drowsiness, confusion, or respiratory depression.
Tailoring the Sedative Plan
In patients with compensated cirrhosis (where liver function is relatively preserved), anaesthetic requirements may not differ much. But in decompensated cases, even small doses of midazolam or propofol could tip the balance.
This is where your anaesthetist’s expertise matters. Instead of using systemic sedatives, they may rely on topical anaesthetic agents and keep systemic medications to an absolute minimum. Some clinics may also pre-emptively reduce any preoperative oral medications that are hepatically cleared.
Avoiding Hepatic Encephalopathy Triggers
Another concern is hepatic encephalopathy – a state of confusion or altered consciousness caused by toxin build-up in the brain due to impaired liver detoxification. Surgery, dehydration, and certain medications (like benzodiazepines or opioids) can precipitate an episode.
To reduce this risk, anaesthetists may avoid certain drug classes altogether or opt for alternatives with less hepatic metabolism. You may also be advised to adjust your diet and avoid protein-heavy meals around the time of surgery.
Healing and Recovery: What to Expect When Liver Function Is Compromised
Liver cirrhosis not only affects your blood and drug metabolism – it also influences your body’s ability to repair itself. The liver helps regulate inflammation, manage infections, and supply nutrients necessary for healing. If it’s impaired, recovery can be delayed and complications may be more likely.
Watch for Signs of Postoperative Bruising and Delayed Wound Healing
Even though cataract incisions are tiny, cirrhotic patients may experience more extensive bruising or subconjunctival haemorrhage than average. While this looks dramatic, it’s usually not dangerous – just slower to clear.
Your eye surgeon might delay restarting blood-thinning medications (if you’re on any) or suggest cold compresses in the early postoperative period to limit bruising. You’ll also be closely monitored for any signs of delayed epithelial healing or increased inflammation.
Risk of Infection: Keeping an Eye on Immunity
Cirrhosis can subtly suppress your immune system, increasing your susceptibility to infections – including endophthalmitis, a rare but serious eye infection. That’s why prophylactic antibiotic eye drops and proper hygiene are particularly important in cirrhotic patients.
In some cases, surgeons may avoid using antibiotic eye drops that are heavily metabolised by the liver, and instead choose safer alternatives with a renal clearance route.
Anticipating Drug Interactions: Antibiotics, Diuretics, and More

Let’s not forget that many patients with cirrhosis are already on medications – such as diuretics for fluid retention or beta-blockers for portal hypertension. Adding new drugs post-surgery can lead to interactions or even toxicity if not carefully chosen.
Avoiding Nephrotoxic Antibiotics
Some antibiotics commonly used after cataract surgery – like aminoglycosides – can stress the kidneys, especially if you’re also on diuretics. Others, such as macrolides or fluoroquinolones, may prolong QT intervals or cause liver enzyme elevation.
Your ophthalmologist will usually opt for topical antibiotics that stay local to the eye with minimal systemic absorption. But even these aren’t risk-free in cirrhotics, especially those with underlying kidney issues or electrolyte imbalances.
Adjusting Your Usual Medications Around Surgery
If you’re taking diuretics like spironolactone or furosemide, you may be advised to withhold them on the day of surgery to reduce dehydration risk. Beta-blockers may be continued unless they cause symptomatic bradycardia or hypotension. Always follow your hepatologist’s guidance here.
Communication Is Key: Coordinating With Your Liver Specialist
Cataract surgery doesn’t happen in isolation – it’s essential that your eye surgeon, anaesthetist, and liver consultant are all in the loop. Ideally, your liver team will send a summary of your most recent labs, medication list, and any cirrhosis-related complications that may influence the surgery.
This multidisciplinary approach is what makes cataract surgery not only safer but smoother. If you’ve had variceal bleeds, episodes of encephalopathy, or recent hospital admissions, those details help the ophthalmology team plan accordingly.
You may also need special arrangements for transport, hydration, and monitoring post-op, especially if you live alone or far from the clinic.
Setting Realistic Expectations for Vision and Recovery
With careful planning, most patients with liver cirrhosis can expect a good visual outcome after cataract surgery. That said, your recovery might be a bit slower, and some postoperative symptoms – like blurry vision or eye redness – might take longer to resolve.
Don’t Rush the Healing
Be patient with the healing process. Your body might be a little slower to clear inflammation or reabsorb haemorrhages. Follow all the aftercare instructions closely, and attend every follow-up appointment – even if your eye feels fine.
Plan for a Support System
If your cirrhosis causes fatigue, weakness, or cognitive symptoms, it’s wise to have someone accompany you to your appointments and help with post-op drops and meals. Setting up support in advance can make all the difference.
Frequently Asked Questions (FAQs)
- Can I have cataract surgery if I have liver cirrhosis?
Yes, you can. Many people with cirrhosis successfully undergo cataract surgery. However, your surgeon will need to take extra precautions to account for bleeding risks, medication metabolism issues, and slower healing. It’s essential that your liver team is involved in the planning process. - Will I need to stop any of my regular liver medications before the surgery?
You may be asked to stop or adjust certain medications, like diuretics, before surgery to prevent dehydration or low blood pressure. Blood thinners may also be temporarily paused depending on your bleeding risk. These decisions will be made in coordination with your liver specialist and surgeon. - What type of anaesthesia is safest for patients with cirrhosis?
Local anaesthesia – usually via eye drops or a small injection – is generally safest. It avoids the liver having to metabolise systemic sedatives and reduces the risk of complications like hepatic encephalopathy. In most cases, general anaesthesia is avoided unless absolutely necessary. - Does liver disease make the healing process slower after cataract surgery?
Yes, it can. The liver plays a role in wound healing and immune response, so recovery might take a bit longer if you have cirrhosis. You may also experience more bruising or subconjunctival bleeding than usual, though this often looks worse than it feels. - Are there any specific antibiotic eye drops I should avoid?
Most antibiotic drops used after cataract surgery are topical and not heavily metabolised by the liver. However, your surgeon may avoid those that are known to stress the kidneys or interfere with other liver-related medications. They’ll choose the safest option based on your full medical history. - How can I reduce the risks before my cataract operation?
Make sure your liver condition is as stable as possible beforehand. Attend your pre-op assessments, share all medications and recent lab results with your eye team, and follow any dietary or medication instructions they give you. Staying well hydrated and supported at home will also help with recovery. - Will I get the same visual improvement as someone without liver disease?
Most patients with cirrhosis still enjoy a noticeable improvement in vision after cataract surgery. Your final outcome may depend on other factors, such as general health or any existing retinal problems, but many people report excellent results. - Should I have any special blood tests done before cataract surgery?
Yes, if you have liver cirrhosis, your medical team will likely check your INR (a measure of how well your blood clots), platelet count, and liver function tests before surgery. These results help the surgical team plan safely, especially when deciding on the type of anaesthesia and whether any clotting support might be needed before the procedure. - Will I need to stay overnight in hospital after cataract surgery if I have cirrhosis?
In most cases, cataract surgery is a day procedure, even for patients with cirrhosis. However, if your liver disease is advanced or you’re at risk of complications like confusion (hepatic encephalopathy), your doctor may recommend short-term observation or an overnight stay just to be cautious. This decision will be made based on your individual condition and support system at home. - Is there a higher risk of cataract surgery failing if I have liver cirrhosis?
Not necessarily. The surgery itself is technically the same, and your risk of failure isn’t higher just because of cirrhosis. However, certain complications like prolonged healing, more visible bruising, or a slightly higher infection risk can occur, so your eye team will take extra steps to minimise these risks and ensure the best possible outcome. - Could portal hypertension affect my eye surgery?
Yes — if your cirrhosis includes portal hypertension with varices, your bleeding risk during surgery is higher. Your surgeon may take additional steps like gentle cauterisation of small vessels and close intra‑operative observation to reduce bleeding complications. - Are there any signs after surgery that should prompt me to contact my doctor?
Definitely. If you notice increasing eye pain, persistent redness, sudden vision loss, or ongoing bleeding beneath the conjunctiva (especially if accompanied by fever), contact your ophthalmologist immediately. These could be early signs of infection or other complications requiring prompt treatment. - Will I need extra follow-up after surgery because of my liver condition?
Probably yes — even if your recovery seems smooth, your eye team may schedule a few extra check-ups to monitor healing, ensure infection doesn’t develop, and confirm that bruising and inflammation are resolving as expected.
Final Thoughts: Cataract Surgery Is Still an Option – With the Right Precautions
Having liver cirrhosis doesn’t mean you can’t have cataract surgery. It just means the surgical team needs to approach your case a bit differently. By addressing your coagulation status, tailoring your anaesthetic plan, and carefully selecting medications, they can minimise your risks and help you achieve clearer vision safely.
Always make sure your eye surgeon knows about your liver condition early in the process, and never hesitate to ask questions. With the right team around you, cataract surgery can be a safe, life-improving procedure – even with cirrhosis in the background.
References
- Schuppan, D. & Afdhal, N.H. (2008) ‘Liver cirrhosis’, The Lancet, 371(9615), pp. 838–851. Available at: https://www.sciencedirect.com/science/article/pii/S0140673608603839 (Accessed: 25 June 2025).
- Tripodi, A. & Mannucci, P.M. (2011) ‘The coagulopathy of chronic liver disease’, New England Journal of Medicine, 365(2), pp. 147–156. Available at: https://www.nejm.org/doi/full/10.1056/NEJMra1011170 (Accessed: 25 June 2025).
- Butterworth, R.F. (2003) ‘Hepatic encephalopathy: a central neuroinflammatory disorder?’, Hepatology, 38(3), pp. 518–521. Available at: https://aasldpubs.onlinelibrary.wiley.com/doi/full/10.1053/jhep.2003.50320 (Accessed: 25 June 2025).