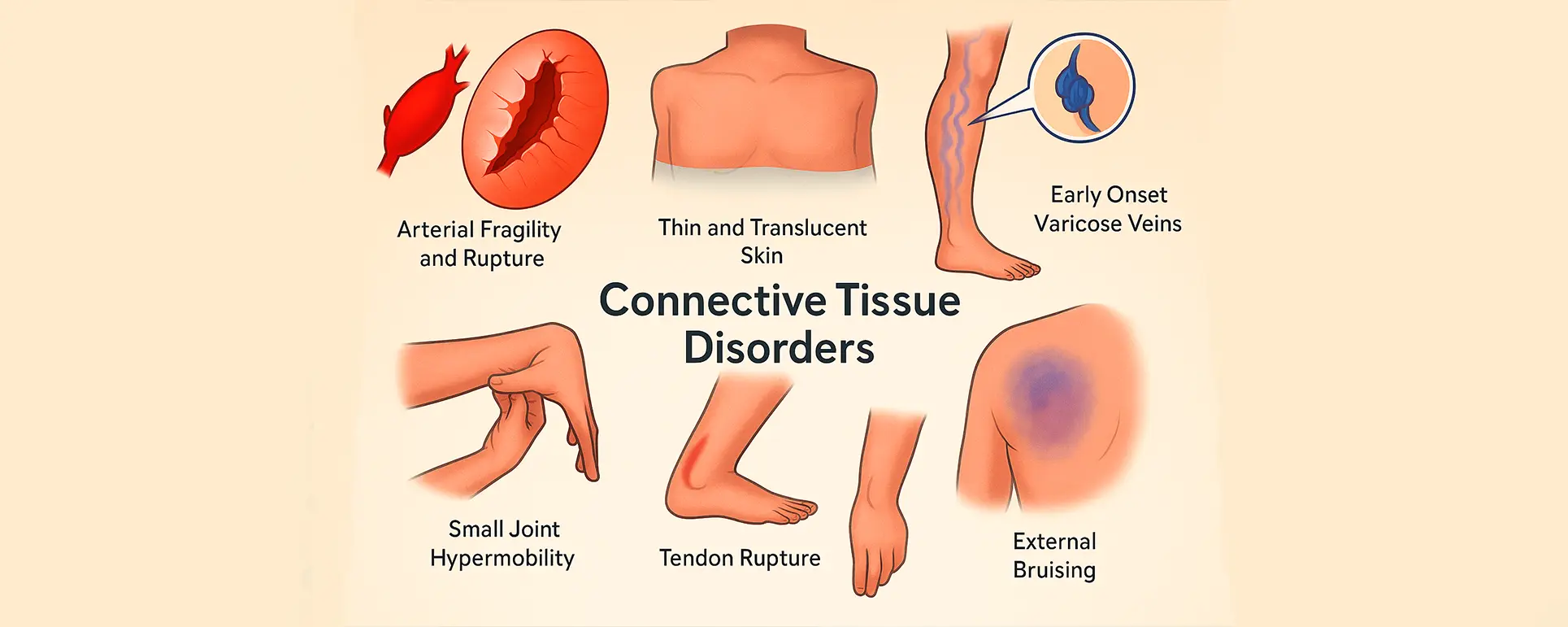
If you or someone you know has a connective tissue disorder like Marfan syndrome, Ehlers-Danlos, or homocystinuria and are facing cataract surgery, you’re not alone in feeling a bit overwhelmed. These conditions don’t just affect the joints and skeleton—they can complicate even routine eye surgeries in ways that demand extra attention and precision. In this article, we’re going to take a closer look at how cataract surgery changes when you’re dealing with systemic connective tissue disease, and what surgeons do to plan for safe and successful outcomes.
Understanding the Role of Connective Tissue in the Eye
The eye might seem like a small organ, but it’s a highly intricate structure, and many of its parts rely on healthy connective tissue to work properly. One of the most important components here is the zonules of Zinn—those fine, fibrous strands that hold the lens in place. If those zonules are weakened, stretched, or broken, as often happens in connective tissue disorders, the lens can shift or become partially dislocated (a condition known as lens subluxation).
In patients with Marfan syndrome or similar conditions, the elasticity and strength of connective tissue are compromised. This fragility is systemic, which means every structure made of collagen or fibrillin is potentially at risk—including the supporting fibres around your lens. As a result, the zonules may be unable to keep the lens centred and stable, making cataract surgery more complex.
Marfan Syndrome and the Ocular System: A Closer Look
Marfan syndrome is a genetic disorder that affects the body’s connective tissue, particularly fibrillin-1. It’s often recognised by its impact on the cardiovascular system, but the eyes are also significantly affected. Up to 60% of people with Marfan syndrome develop ectopia lentis—where the lens becomes displaced or even mobile within the eye.
When cataracts develop on top of a subluxated lens, surgeons must account for a double challenge: removing the cloudy lens while also dealing with the fact that it may not be securely held in place. The risk of the lens moving or collapsing during surgery is much higher than normal, and this can raise the risk of complications such as vitreous loss or IOL (intraocular lens) malposition.
What Makes Cataract Surgery Different in These Patients?
So, what does all this mean when it comes to the operating theatre? First, there’s a greater need for detailed pre-operative planning. Your surgeon will want to assess the degree of lens subluxation and zonular weakness using high-resolution imaging, often with ultrasound biomicroscopy or anterior segment OCT. This helps them visualise how much support the natural lens still has and whether additional devices will be needed to stabilise the IOL.
In many cases, standard phacoemulsification techniques won’t be suitable without modification. The capsulorhexis—the circular opening made in the lens capsule—must be approached with great care, as pulling forces can easily cause further zonular dehiscence. To mitigate this, surgeons may use capsule stabilising devices such as capsular tension rings (CTRs), segments, or sutured IOLs.
Zonular Weakness: Recognising and Managing It
Zonular instability is the hallmark issue in connective tissue disorders when it comes to cataract surgery. But how does a surgeon detect it, and what do they do about it?
Sometimes it’s obvious. If the lens has visibly shifted or trembles with eye movement (a phenomenon known as phacodonesis), you can assume zonular support is compromised. Other times, the problem becomes apparent only once surgery is underway.
Intraoperative tools like capsular hooks or CTRs can help redistribute tension and prevent the bag from collapsing. But in severe cases—especially when zonular loss affects more than 4 clock hours of the capsule—the surgeon might choose to bypass the capsule entirely and implant an anterior chamber IOL, or one fixated to the sclera or iris. These advanced techniques allow for lens replacement even when the natural support system has failed.
Surgical Planning: Timing and Teamwork Matter
Because Marfan and other connective tissue conditions often involve multiple systems, cataract surgery isn’t just an ophthalmological concern. Collaboration with cardiologists, anaesthetists, and sometimes geneticists may be needed—especially in cases where general anaesthesia is considered or when anticoagulants are in play.
There’s also the question of timing. In some patients, early surgery may be indicated not just because of vision loss from the cataract, but to pre-empt further lens dislocation or secondary complications like glaucoma. In others, surgery might be delayed to reduce anaesthetic risks or to coordinate with cardiovascular procedures.
Ultimately, every case is individual. But what’s consistent is that these surgeries are rarely “routine” and benefit from being done at centres familiar with the complexities of systemic connective tissue disorders—such as the London Cataract Centre, where surgeons routinely manage high-risk, structurally complex eyes.
Paediatric Considerations: When Cataracts Affect Younger Patients

Marfan syndrome, Stickler syndrome, and other connective tissue disorders often present in childhood or adolescence, and cataracts in these patients can be congenital or early-onset. Operating on a paediatric eye poses its own set of challenges, not just technically but developmentally.
Children with connective tissue disorders are more likely to experience amblyopia (lazy eye) if cataracts aren’t addressed early. However, lens implantation in growing eyes must be approached carefully. Surgeons may opt for aphakic correction (leaving the eye without a lens and correcting with glasses or contact lenses) initially, postponing IOL implantation until the eye has stabilised.
What’s more, paediatric eyes with weak zonules are at higher risk of capsular contraction or IOL dislocation post-surgery. Long-term follow-up is critical, often involving multiple disciplines including orthoptists, paediatricians, and genetic counsellors.
The Role of Genetic Testing and Family Screening
Cataracts in patients with known connective tissue disorders may prompt screening in family members, particularly in inherited conditions like Marfan or homocystinuria. Genetic testing can confirm diagnoses and help guide future ophthalmic surveillance. This is especially important because ocular signs like ectopia lentis or axial myopia often precede more dangerous cardiovascular complications.
If you’ve been diagnosed with one of these disorders and are showing signs of early cataract or lens instability, it’s worth having your first-degree relatives screened. Many clinics now offer combined eye and genetic counselling services to make this process more streamlined.
Postoperative Care and Long-Term Follow-Up
Recovery after cataract surgery in these patients can be less predictable. Because the lens support structures are inherently fragile, there’s an increased risk of late IOL dislocation, capsular fibrosis, and even retinal detachment.
That’s why your follow-up schedule will likely be more frequent than for a standard cataract patient. Expect a closer watch on IOL position, intraocular pressure, and posterior capsule opacification (which can develop earlier in eyes with abnormal lens behaviour). YAG laser capsulotomy may still be used when necessary, but it must be approached with caution to avoid destabilising the IOL.
It’s also not unusual for further surgical interventions to be required down the line. The earlier issues are spotted, the better the chance they can be corrected with minimal disruption to your vision.
Anaesthetic Considerations: Not All Sedation Is Equal
People with Marfan syndrome may have cardiovascular vulnerabilities like aortic root dilation, arrhythmias, or mitral valve prolapse. These raise specific concerns for anaesthesia. For some patients, local anaesthesia with minimal sedation is safest. For others—particularly children or those with poor cooperation—general anaesthesia might be required, but only under the watch of an experienced anaesthetist with access to cardiovascular support.
This again highlights the importance of having your cataract surgery in a multidisciplinary environment, where both eye surgeons and anaesthetists understand the broader implications of systemic disease.
Future Directions in Surgical Tools and Techniques

Research is ongoing into more adaptive IOLs and lens-fixation systems that can accommodate patients with little or no zonular support. Advances in femtosecond laser-assisted cataract surgery (FLACS) may allow for even more precise, less traumatic surgery in these eyes. However, FLACS is not without its own set of concerns in connective tissue disorders, particularly when corneal stability is affected.
In parallel, new capsule support devices and hybrid IOL anchoring systems are being tested in clinical trials. These could dramatically improve long-term outcomes and reduce the rate of IOL-related complications in these complex eyes.
Frequently Asked Questions (FAQs)
1. Why is cataract surgery riskier in patients with Marfan syndrome?
Cataract surgery is riskier in people with Marfan syndrome due to the fragility of the zonular fibres that hold the lens in place. These fibres are often weak or stretched, increasing the chances of lens subluxation or dislocation during surgery. As a result, surgeons may need to use specialised devices, such as capsular tension rings or alternative IOL fixation techniques, to stabilise the lens and prevent complications.
Additionally, patients with Marfan syndrome may also have cardiovascular issues, which complicate anaesthetic management. The surgical team must coordinate closely to plan the safest possible procedure, tailoring the approach to each patient’s specific risks and anatomy.
2. What is ectopia lentis, and how does it affect cataract surgery?
Ectopia lentis refers to the displacement or subluxation of the natural lens inside the eye. In connective tissue disorders like Marfan syndrome or homocystinuria, this occurs because the zonules (which suspend the lens) are abnormally weak. In cataract surgery, ectopia lentis can make lens removal and IOL placement more challenging, as the lens may not be stable or centred.
Surgeons may need to modify the procedure by using capsular support devices or implanting the IOL outside the capsule. The aim is to ensure that the replacement lens remains securely positioned and that vision is restored safely.
3. Can children with connective tissue disorders safely undergo cataract surgery?
Yes, but it requires careful planning. Children with connective tissue disorders often develop cataracts at a younger age and may also have associated ocular conditions such as high myopia or glaucoma. Paediatric cataract surgery in these cases involves greater complexity due to lens instability and the ongoing growth of the eye.
Surgeons may sometimes delay IOL implantation and use alternative visual correction methods until the child’s eye matures. Postoperative follow-up is crucial to monitor visual development and intervene early if complications like amblyopia or lens dislocation arise.

4. How is anaesthesia managed for patients with Marfan syndrome during cataract surgery?
Anaesthesia in Marfan patients is carefully chosen based on cardiovascular status. Because of the risk of aortic dilation or arrhythmias, many patients are best served with local anaesthesia and minimal sedation. However, in children or those unable to cooperate, general anaesthesia might be necessary and should only be administered by an anaesthetist familiar with connective tissue disorders.
A full cardiovascular work-up may be done preoperatively to assess risk, and intraoperative monitoring will often be more intensive than in standard cases.
5. Are there long-term risks after cataract surgery in people with connective tissue diseases?
Yes, the risks don’t end once surgery is over. Patients with weak zonules may experience delayed dislocation of the IOL or capsule contraction, which can lead to visual disturbances. There’s also an elevated risk of retinal detachment and earlier development of posterior capsule opacification.
That’s why long-term follow-up is essential. Regular check-ups ensure early detection of any shift in IOL position or pressure changes, allowing timely intervention to maintain vision.
6. What are capsular tension rings, and why are they used in connective tissue disorders?
Capsular tension rings (CTRs) are circular devices made of flexible plastic that are inserted into the lens capsule during cataract surgery. Their main job is to stabilise the capsule when the zonular fibres are weak or damaged—exactly the scenario often seen in Marfan syndrome, Ehlers-Danlos syndrome, and similar conditions. By distributing tension evenly around the capsule, CTRs help prevent capsular collapse and keep the intraocular lens (IOL) centred postoperatively.
In more severe cases, modified CTRs with fixation points can be anchored to the sclera to provide even more support. These devices are key in allowing the surgeon to safely implant an IOL even when the natural support structure is compromised.
7. Is femtosecond laser cataract surgery recommended for patients with connective tissue disease?
Femtosecond laser-assisted cataract surgery (FLACS) can offer advantages for patients with connective tissue disorders by creating highly precise incisions and a centred, circular capsulotomy with minimal mechanical stress. This precision can reduce the risk of worsening zonular damage during the procedure. However, FLACS may not be suitable for everyone, especially if corneal abnormalities or small eye anatomy are present—features that can also be part of systemic connective tissue syndromes.
Surgeons will evaluate whether the benefits of using the laser outweigh any limitations in your specific case. In experienced hands, FLACS can enhance surgical safety and outcomes for patients with fragile ocular structures.
Final Thoughts: A Surgery That Demands Individualisation
Cataract surgery in patients with Marfan syndrome and other connective tissue diseases is not a one-size-fits-all procedure. It’s a tailored operation that requires not only surgical finesse but also a deep understanding of systemic disease, preoperative anatomy, and long-term planning.
If you’re facing surgery and live with one of these conditions, make sure you’re treated at a centre equipped to handle it. At the London Cataract Centre, we routinely manage structurally complex eyes and work closely with cardiologists and anaesthetists to ensure your care is both safe and effective. You only get one set of eyes. Choosing the right team for your private cataract surgery makes all the difference.
References
- Konradsen, T.R. and Zetterström, C., 2013. Subluxation of the lens and cataract surgery: preoperative assessment and surgical strategies. Acta Ophthalmologica, 91(7), pp. 641–646. Available at: https://onlinelibrary.wiley.com/doi/full/10.1111/aos.12086
- Maumenee, I.H., 1981. The eye in the Marfan syndrome. Transactions of the American Ophthalmological Society, 79, pp. 684–733. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1312152/
- Chandra, A. and Charteris, D.G., 2014. Molecular pathogenesis and management strategies of ectopia lentis. Eye, 28(2), pp. 162–168. Available at: https://www.nature.com/articles/eye2013256
- Grzybowski, A. and Kanclerz, P., 2018. Capsular tension rings and segments in cataract surgery for lens subluxation. Journal of Cataract and Refractive Surgery, 44(5), pp. 665–666. Available at: https://www.jcrsjournal.org/article/S0886-3350(18)30133-5/fulltext
- Black, G.C. and Mullaney, P.B., 2021. Management of paediatric cataract in connective tissue diseases. In: Pediatric Cataract: A Global Perspective. Springer, pp. 141–152.