If you’ve been told you have astigmatism and cataracts, chances are your ophthalmologist has mentioned something called a “toric intraocular lens” or toric IOL. These lenses are specifically designed to tackle both problems in one go: they replace the cloudy lens during cataract surgery and correct the irregular curvature of your cornea. Sounds like a win-win, right?
But the real question isn’t just whether they work on day one—it’s how well they hold up over time. Do toric lenses remain stable? Is your vision still clear years later? Are patients actually happy long-term? In this deep dive, we’ll walk you through what long-term research shows about the performance of toric IOLs. From rotational stability and refractive accuracy to patient satisfaction and quality of life, we’re covering it all.
What Exactly Are Toric IOLs, and Why Do They Matter?
Let’s start with the basics. A toric intraocular lens is a premium lens implant used during cataract surgery to correct astigmatism. Unlike standard IOLs, which only address nearsightedness or farsightedness, toric lenses have different powers in different meridians of the lens to counter the uneven curvature of the cornea.
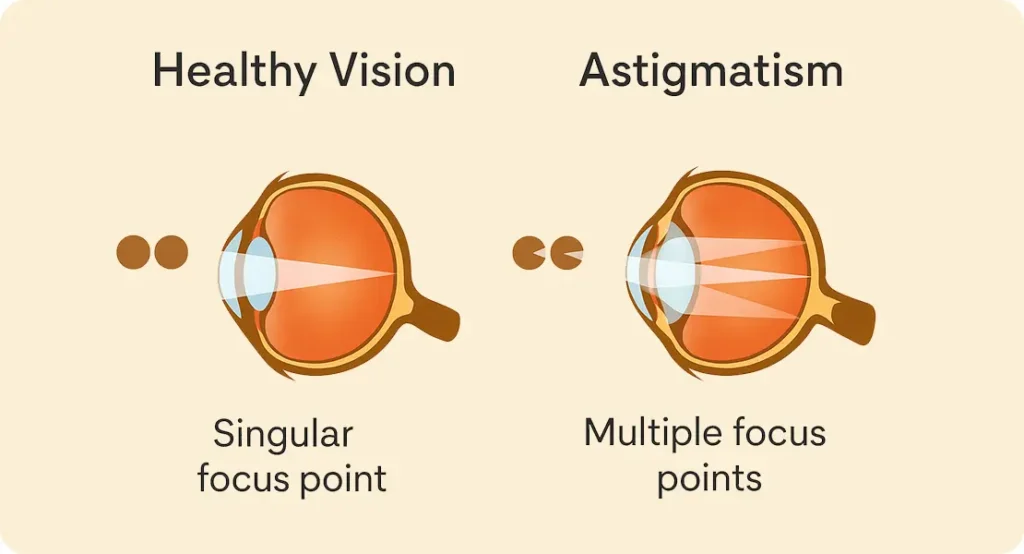
Astigmatism, in simple terms, means your eye isn’t perfectly round. Instead of a smooth, even dome like a football, your cornea might be more like a rugby ball—curved more in one direction than the other. This irregularity causes light to scatter as it enters the eye, leading to blurred or distorted vision. Toric lenses are designed to neutralise that asymmetry.
Now here’s the catch: these lenses must be positioned at a very specific angle in your eye. Even a few degrees off can reduce their effectiveness significantly. So when we talk about long-term performance, we’re really asking, “Does the lens stay put? And does it keep delivering crisp vision?”
Rotational Stability: The Make-or-Break Factor
This is arguably the most critical metric for toric lenses. Since the correction of astigmatism depends on the precise alignment of the lens, any rotation over time can compromise visual outcomes.
Early Postoperative Rotation
Let’s look at what typically happens after surgery. Most rotation, if it occurs, happens within the first 48 hours. This is when the eye is still healing and the lens is settling into place. Surgeons try to compensate for this by slightly over-rotating the lens during placement based on expected movement.
In most modern studies, about 90% of toric lenses rotate less than 5 degrees postoperatively—a threshold that’s usually considered clinically insignificant. For reference, a 10-degree rotation can reduce effectiveness by about one-third, and a 30-degree shift essentially nullifies the correction.
Long-Term Rotational Outcomes
Longitudinal studies tell an encouraging story. In a 5-year follow-up study involving over 400 patients, researchers found that toric lenses rotated an average of just 1.5 degrees after the initial healing period. Another study published in Ophthalmology followed patients for over a decade and found minimal lens movement beyond the first year. The key takeaway? If your toric IOL is stable at one month, chances are it will stay that way for years.
Design Improvements Over Time
Not all toric IOLs are built the same. Modern designs include haptic (the supporting arm) improvements that anchor the lens more securely. Brands like the AcrySof IQ Toric and TECNIS Toric have shown particularly strong rotational stability in long-term studies. These lenses often feature textured surfaces and refined shapes to better “grip” the lens capsule.
Long-Term Refractive Outcomes: Do They Hold Up?
Okay, so the lens stays put—but what about your actual vision?
Predictability of Astigmatic Correction
Toric intraocular lenses are highly regarded for their ability to deliver accurate and predictable correction of astigmatism during cataract surgery. Unlike incisional techniques, which can be influenced by healing responses and corneal biomechanics, toric IOLs provide a built-in refractive solution that, when placed correctly, significantly reduces residual astigmatism. Their success hinges on careful preoperative measurements, including corneal topography and biometry, to determine the correct power and axis alignment. When this planning is done meticulously, the results are often impressively precise.
That said, long-term predictability isn’t solely determined by what happens during surgery. The eye itself continues to change subtly with age, which can influence refractive outcomes. The curvature of the cornea can shift slightly over time, and natural ageing processes may alter the ocular surface. In addition, posterior capsule opacification (PCO)—a common occurrence in the years following cataract surgery—can cause visual symptoms that mimic refractive error, even though the lens itself hasn’t moved. Despite these variables, long-term studies show that the correction provided by toric IOLs holds up well in the majority of cases.
One 7-year observational cohort study found that approximately 85% of patients remained within ±0.50 dioptres of their intended astigmatic correction, which speaks volumes about the durability of these lenses. This level of stability is considered excellent, especially when you factor in the normal biomechanical and anatomical shifts that happen in the ageing eye. It means that most patients can continue to enjoy sharp, distortion-free vision for many years after surgery without needing additional refractive intervention.
Impact of Secondary Procedures
One of the most common secondary procedures following cataract surgery is a YAG laser capsulotomy, typically performed to treat posterior capsule opacification (PCO). PCO occurs when the thin membrane behind the intraocular lens becomes cloudy, which can blur vision and mimic cataract-like symptoms. The YAG procedure involves using a focused laser to create a small opening in this membrane, allowing light to pass through clearly again. It’s quick, painless, and highly effective—but naturally, patients with toric IOLs may wonder if this laser pulse could disturb their lens alignment.
Fortunately, with newer toric lens designs, the risk of displacement during a YAG laser capsulotomy is minimal. Manufacturers have made significant advances in haptic design and lens surface texture to improve fixation within the capsular bag. These enhancements help the lens stay exactly where it was placed, even when the surrounding tissue is altered by a laser pulse. In the vast majority of cases, visual clarity improves post-YAG without any compromise to astigmatic correction, making it a safe procedure for patients with toric implants.
However, there have been isolated reports where a slight rotational shift was observed following a YAG procedure, particularly in older lens models or in eyes with unusual anatomy. This has prompted many ophthalmologists to make it standard practice to assess lens alignment after performing the laser treatment. If any significant rotation is detected—which is rare—it can usually be corrected with a minor surgical adjustment. Being aware of this possibility allows patients to receive timely intervention if needed, preserving the long-term effectiveness of their toric IOL.
Visual Acuity and Quality of Life: What Patients Say Years Later
It’s one thing to measure degrees of rotation or refractive error, but what really matters to most people is how well they can see—and how they feel about it.
Uncorrected Visual Acuity (UCVA)
Most long-term studies report excellent uncorrected distance vision in patients with toric lenses. One 10-year study found that 78% of patients still had 6/9 vision or better without glasses. That’s especially impressive considering the natural progression of presbyopia and other age-related issues.
Spectacle Independence
Many patients report reduced dependence on glasses post-surgery. Though toric lenses don’t correct presbyopia (age-related near vision loss), they significantly reduce the need for glasses for distance tasks. For some, that means driving, watching TV, or even recognising faces in social settings becomes easier—without reaching for specs.
Patient-Reported Outcomes
So what do people actually say about their experience? Satisfaction surveys conducted years after surgery consistently show high approval ratings. In a multi-centre trial with over 1,000 patients, 89% said they would choose the same lens again. Common praises included better contrast sensitivity, reduced glare at night, and greater confidence during daily activities.
How Toric IOLs Compare to Other Astigmatism Solutions
If you’re still deciding whether toric IOLs are the best fit, it helps to compare them to alternatives like limbal relaxing incisions (LRIs) or laser-assisted astigmatic keratotomy (AK).

Limbal Relaxing Incisions vs Toric Lenses
Limbal relaxing incisions (LRIs) have long been used as a straightforward method to reduce corneal astigmatism during cataract surgery. The technique involves making small, strategically placed cuts at the periphery of the cornea to relax its curvature, thereby evening out the corneal shape. While LRIs are easy to perform and relatively low in cost, they rely heavily on manual execution and corneal wound healing patterns, which can vary from patient to patient. As a result, the precision of the outcome is less predictable, especially in patients with moderate to high degrees of astigmatism.
One of the main drawbacks of LRIs is their tendency to regress over time. Although patients might initially enjoy an improvement in vision, the cornea can gradually return to its original shape, particularly if the incisions were shallow or not placed at the optimal location. Environmental factors, age-related changes, and the natural biomechanics of the cornea can all influence long-term stability. This means that while LRIs may provide a short-term benefit, they often fall short of delivering consistent, lasting astigmatism correction in the years following surgery.
In contrast, toric intraocular lenses offer a more permanent and reliable solution. By embedding astigmatic correction directly into the lens implanted during cataract surgery, toric IOLs address the root of the problem with a high level of precision. They don’t rely on the cornea’s healing response, which makes their outcomes more stable over time. For patients with astigmatism greater than 1.0 dioptre, toric lenses are widely regarded as the better long-term option, offering superior visual outcomes with less risk of regression or variability.
Laser-Assisted AK vs Toric Lenses
Laser-assisted astigmatic keratotomy (AK) builds on the concept of LRIs but uses a femtosecond laser to create more precise and repeatable incisions. The key advantage of laser-assisted AK is its enhanced control: the depth, length, and orientation of the incisions can be programmed to match the patient’s exact corneal topography. This significantly reduces the variability associated with manual techniques. It also offers an appealing middle ground for patients who aren’t suitable for toric lenses or prefer not to opt for a premium IOL.
That said, while laser AK improves on manual LRIs, it still doesn’t match the consistency of toric IOLs for most patients. The effectiveness of laser incisions can still vary due to corneal biomechanical responses, and they are generally less effective in treating higher levels of astigmatism. In addition, the correction achieved through incisional methods—laser or otherwise—is not always permanent. There’s still the possibility of partial regression over time, particularly in younger or more active patients whose corneas may continue to change shape after surgery.
Toric lenses avoid these pitfalls by providing a refractive correction that remains fixed within the eye. Since the astigmatism correction is built into the lens, and not reliant on the cornea’s response to an incision, the outcomes tend to be more predictable and long-lasting. While the initial cost of toric IOLs is often higher, especially in private settings, their superior long-term performance makes them a compelling investment for many patients. For those seeking the most reliable option for correcting significant astigmatism during cataract surgery, toric lenses consistently come out ahead in terms of both clinical data and patient satisfaction.
Key Factors That Influence Long-Term Outcomes
So what determines how well your toric IOL performs years down the line? Here are a few critical considerations:
Accurate Biometry and Planning
Precise pre-operative measurements—especially of the corneal curvature and axis—are crucial. Modern devices like swept-source OCT biometry and topography-guided planning tools have made a big difference in this area. The more accurate the data going in, the better the result coming out.

Surgical Technique
It’s not just about the lens; it’s about how it’s placed. Studies have shown that surgeon experience and technique significantly impact long-term alignment. Intraoperative guidance systems, like Callisto or VERION, can also improve accuracy.
Eye Anatomy
Some eyes are simply more prone to rotation. Factors such as a large capsular bag or unusually long axial length can increase the likelihood of lens movement. Fortunately, these risks can often be identified and mitigated during planning.
Limitations and What the Studies Don’t Always Capture
Of course, no treatment is perfect. While toric IOLs offer excellent long-term results for many, they aren’t without limitations.
Residual Astigmatism
In a minority of cases, patients still experience mild residual astigmatism. This might be due to lens misalignment, healing variability, or underestimation of posterior corneal astigmatism. Thankfully, most of these cases can be managed with glasses or touch-up laser procedures.
Cost and Access
Toric IOLs are considered premium lenses, which means they usually come with an extra cost and are not routinely covered by NHS cataract services. For some, this makes them less accessible—even if they offer superior outcomes.
The Ageing Eye
Lastly, the lens might be stable, but the rest of the eye keeps changing. Dry eye, macular degeneration, and glaucoma can still affect overall vision regardless of the IOL. It’s important to keep up with regular eye exams even after cataract surgery.
Final Thoughts: Are Toric IOLs Worth It Long-Term?
If you’re dealing with both cataracts and astigmatism, toric IOLs are more than just a convenient solution—they’re a long-term investment in better vision. The research overwhelmingly supports their effectiveness in maintaining rotational stability, preserving refractive accuracy, and keeping patients happy years after surgery. If you would like to learn more about how toric lenses can help you correct astigmatism and cataracts, you can get in touch with us at the London Cataract Centre to discuss your situation with one of our expert cataract surgeons.
But like any medical decision, success depends on proper planning, surgical skill, and individual anatomy. The good news? If your eye is a good candidate and the surgery is well-executed, the odds are heavily in your favour.
So if you’re weighing up your lens options, here’s the takeaway: toric IOLs don’t just work—they stay working. And that might just make all the difference in how clearly you see the world, for years to come.
References
- Ferreira, T.B., Marques, E.F., Rodrigues, A. and O’Neill, J.G., 2017. Long-term rotational stability and visual outcomes of a single-piece toric intraocular lens. Clinical Ophthalmology, 11, pp.1349–1355. Available at: https://www.dovepress.com/long-term-rotational-stability-and-visual-outcomes-of-a-single-piece–peer-reviewed-article-OPTH [Accessed 15 May 2025].
- Kaur, M., Titiyal, J.S., Raj, A. and Agarwal, T., 2018. Factors affecting the outcome of toric intraocular lenses: A review. Asia-Pacific Journal of Ophthalmology, 7(5), pp.339–349. Available at: https://journals.lww.com/apjoo/Fulltext/2018/09000/Factors_Affecting_the_Outcome_of_Toric_Intraocular.7.aspx [Accessed 15 May 2025].
- Hirnschall, N., Maedel, S., Weber, M., Amir-Asgari, S. and Findl, O., 2014. Rotational stability of a single-piece toric acrylic intraocular lens: a long-term follow-up study. Ophthalmology, 121(1), pp.35–41. https://doi.org/10.1016/j.ophtha.2013.06.017 [Accessed 15 May 2025].
- Visser, N., Bauer, N.J. and Nuijts, R.M., 2013. Toric intraocular lenses: historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. Journal of Cataract & Refractive Surgery, 39(4), pp.624–637.
- Ahmed, I.K., Rocha, G., Slomovic, A.R., 2021. Improving refractive outcomes with toric IOLs: strategies and innovations. EyeWorld, [online]

